CURRENT UNDERSTANDING IN COMMON SURGICAL PROCEDURES FOR THE OPTIMAL ANIMAL PRODUCTION UNDER FIELD CONDITION
Prof (Dr) Md Moin Ansari
University Professor and Head
Department of Veterinary Surgery and Radiology
Bihar Veterinary College Campus,
Bihar Animal Sciences University
Patna-800014, India
Abstract:
Common surgical procedures can be conducted and managed under field condition setting in humane, skilled, and scientific way for the optimal animal production and productivity. Standard tenets of Halsted surgical techniques can be applied to field surgeries in most of the cases. Few compromises critical condition is being performed under anaesthetic, analgesic and aseptic techniques are absolutely required.
Key Words: Animal, Surgery, Field Condition, Wound, Fracture, Abscess, Cow
Introduction
In developing countries, the treatment of wounds poses a significant problem. A wound may be defined as disruption of the cellular or anatomical continuity of the normal organ structure, caused by physical, chemical, mechanical or biological agents. Wound composed of a wall and its contents, contents may be damaged tissue debris and blood clots. Wound healing, has a continuing challenge in rehabilitation/regenerative medicine. Rapid and uncomplicated wound healing, always a primary goal of surgery, is practically desirable for large wounds or wound over vital structures because failure of wound repair is potentially catastrophic. Despite some recent advances in understanding its basic principle, problem in wound healing continues to cause significant morbidity and mortality. Keeping in view the present scenario of filed condition animals, suffer variety of disorders. Most of the recorded surgical affections resulted in high economic losses in the form of treatment cost, damage to hide, hair and wool, low milk and meat production or even death of the affected animals. Affection of teat and udder skin is usually caused by viruses, pyogenic bacteria, necrotizing bacteria or fungi. Lesions may affect the epithelium of the teat orifice, the teat barrel and the udder skin. Viral infections usually cause primary lesions. Bacterial infections may cause primary lesions or be secondary infections of pre-existing viral lesions or trauma. Viral infections vary in severity, infectivity and frequency of occurrence. Inflammation to the teat can be caused by many types of injury including infectious agents and their toxins, physical trauma or chemical irritants. Changes in the pliability of teat tissue caused by congestion or edema may change the resistance of the teat canal to bacterial invasion. Reported that physical injury to the teat might result from chronic mastitis, traumatic hand milking, calves sucking each other and tick bites. The udder and teats are vulnerable to external trauma or injury because of their anatomical location, increase in size of udder and teats during lactation, faulty methods of milking, repeated trauma to the teat mucosa, injury by teeth of calf, unintentionally stepped on teat, paralysis resulting from metabolic disturbances at parturition. Most of surgical procedures of the udder and appendages performed on the bovine are the same adopted on small ruminants and other large species, yet anatomical differences may dictate a suitable modification in operative techniques. The individual’s disorders like abscesses, cysts, hernias, udder and teat affections, intestinal prolapse and atresia ani, ocular affections, urogenital system affections, neoplasms and their scientific management for rural livelihood shall be presented.
- Abscess: is an area of localized suppuration consisting of a defensive wall of connective tissue lined by a “pyogenic membrane” and containing pus. It is a defensive reaction of the tissue to prevent the spread of infectious materials to other parts of the body. In other words, an abscess is a collection of pus contained in a small area walled off from the rest of the body by inflammatory cells and decaying tissues formed by the tissue on the basis of an infectious process (usually caused by bacteria or parasites) or other foreign materials (e.g., splinters, bullet wounds, or injecting needles).
Diagnosis of abscess: An abscess is diagnosed clinically by means of the history and a physical exam, demonstrating a tender mass with overlying erythema (redness). The appearance of considerable numbers of neutrophilic leukocytes in or on a tissue justifies a diagnosis of purulent inflammation. Culturing the abscess material for members of the genera Corynebacterium, Pseudomonas, Streptococcus and Staphylococcus confirms the diagnosis and the causative organism.
Differential Diagnosis: An abscess should be differentiated from a cyst, a haematoma, a synovial distention or an abdominal pain or tumor.
- Abscess: i. Abscess develops acutely after 2-5 days of injury. ii. It is painful and firm at periphery and soft at center. iii. On exploration reveals pus.
- Cyst: i. It is devoid of inflammatory manifestation, ii. Should develop slowly and fluctuate uniformally, iii. It is painless and margins are not firmed (hard), iv. On exploration reveals straws color or serous fluid.
- Haematoma: i. Feels doughy in palpation and crepitates on pressure, ii. It develops immediately after injury and does not points, iii. It is an accumulation of coagulated serum/blood, iv. It is not so painful and margins are not firmed, v. On exploration reveals clotted blood and serum.
- Abdominal hernia: i. It has got a definite hernial ring, ii. Many hernias are reductive/reducible in nature when contents go back and cavity becomes empty, iii. on exploration doesn’t reveals any things (gases and intestinal contents having foul swells)., iv. Never punctured.
- Synovial distention (arthritis/tendinitis): a distended synovial sheath is recognized by its location and by careful palpation. It will take 5 -10 days for development.
- Tumor: i. hard swelling, ii. Growth is not rapid, iii. It is neither hot nor painful, iv. On exploration reveals clotted blood.
- Empyema: Abscesses must be differentiated from empyemas, which are accumulations of pus in a preexisting rather than a newly formed anatomical cavity.
Treatment
Treatment of abscess comprises of:
- Measures to hasten its maturation.
- Abscesses do not generally need to be treated with antibiotics, but they will require surgical intervention (incision and drainage), debridement and curettage.
- The abscess should be inspected to identify if foreign objects are a cause, which may require their removal. Surgical drainage of the abscess (e.g., lancing) is usually indicated once the abscess has developed from a harder serous inflammation to a softer pus stage.
- The treatment is aimed at maturation of abscess and opening the abscess to evacuate its contents. An abscess should not be opened when it is im- mature. If the abscess is not mature the following measure is adopted to hasten the maturation: hot fomentation for 10 minutes in 3-4 times in a day, application of mild rubefacient like Iodine ointment, application of warm poultices, ultrasonic rays and infra red rays
- Once mature, the abscess should be incised at the most dependent part with a knife or a sharp pointed concave bistouries. Generally the incision should be made parallel to the long axis of vessels and nerves running in the area. The site where it is proposed to open and the surrounding area should be cleaned and prepared as for a surgical operation; after shaving and washing the area with soap and water, drying and applying a suitable antiseptic like tincture iodine. A sterilized scalpel may be used to open the abscess. The opening should be at the site where it ‘point’. It should as far as possible be in a ‘dependent portion’ to facilitate drainage. Dependent portion where means a lower are a through which drainage by cavity is possible in the normal position of the If the abscess is not pointing at a dependent portion it is sometimes necessary to make another opening in the dependent portion to provide drainage. This is called a ‘counter opening’. In order to make a first opening a seton needle may be passed through the dependent portion. After wards a ‘seton’ (gauge dipped in antiseptic solution) may be passed through the eye of the order to keep the opening patent. The set on is changed each day after cleaning the abscess cavity. After opening the abscess the contents usually start running. The abscess cavity should be irrigated with hypertonic saline. Afterwards it is packed with set on gauze dipped in tincture iodine. This is intended to destroy any infection remaining therein and also to exert a mild irritant action to stimulate the healing process. The gauze packs are removed after 24 hours and then the abscess cavity is irrigated with a mild antiseptic lotion. The conventional method was to irrigate with a 1 in 500 solution of Acriflavin sulfate as it is a solution, which retains its antiseptic properties even in the presence of pus.
- In modern times many patent antiseptic solution like dettol, savlon etc. are available. Topical application of antiseptic or antibiotics in the form of ointments or dusting powder is indicated if virulent infection is suspected and systemic use of antibiotics may also be necessary in some cases.
- Treatment of chronic abscess is designed on the same line as in case of an acute abscess. The pus may be inspissated when the abscess is longstanding. This necessitates removal with the fingers or a curette. Irritant antiseptic dressing is indicated to promote inflammation and consequent granulation and
- Other modality for abscess treatment.
Herbal treatment: use of various traditional herbal treatments to cure abscess.
Acupressure treatment: use of various locations of acupressure points on the body for abscess disease.
Homeopathy treatment: use of homeopathic remedy for curing abscess.
Magnesium sulfate paste: abscesses a swell as boils and many other collections of pus have been treated via application of magnesium sulfate paste. This works by drawing the infected pus to the surface of the skin before rupturing and leaking out, after this the body will usually repair the old infected cavity. Magnesium sulfate paste is considered a “home remedy” and is not necessarily an effective or accepted medical treatment.
- Cyst: A cyst is a closed/abnormal/ sac having a distinct inner lining of secreting membrane. Or a cyst is a pathological condition which consists of closed cavity having fluid or semifluid contents and will be usually lined by epithelium surrounded by a coat of fibrous tissue of that part in which it is present. Either congenital types as tassel cysts or acquired types as thyroid cysts were reported. Diagnosis usually depends upon clinical history, exploratory puncture and nature of the aspirate, radiographic examination and sometime histopathological examination of the cyst.
Treatment: 1. Puncture and evacuate the contents of cyst by needle or trocar and cannula and inject irritant solution like Tr. Iodine or 5% Carbolic acid to destroy secretory lining and to stimulate granulation tissue for obliteration of the cavity. 2. Surgical incision at lowest point and swap with Tincture Iodine to stimulate granulation tissue formation and obliteration (preferred option). 3. Seton may be used to stimulate granulation tissue formation and obliteration. 4. Surgical excision: intact cyst is carefully dissected and removed from the surrounding tissue in possible cases. Pedunculated cysts of the base of tongue, vagina, or abdominal cavity can be removed by ecraseur to avoid bleeding. Ovariectomy or castration for removal of ovarian or testicular cyst. Hydrocoele can be treated by evacuation of fluid that is followed by castration. Dentigerous cyst can be treated by surgical excision, curetting, cauterization of the sinus, then closure of the wound with establishment of an opening at the lowest point for drainage.
3.Hernia: It is the protrusion of an organ or tissue through congenital or an acquired opening. This opening may be caused by a tear in the abdominal wall or a natural opening like the inguinal canal or femoral canal. Any trauma caused by horn thrust, kick, and violent contact with blunt objects or by an abdominal distension due to pregnancy or straining during parturition may lead to ventral abdominal hernia. However, improper closure of umbilicus at birth due to hypoplasia of the abdominal muscles resulted in umbilical hernia. In addition, outbreaks of umbilical hernias in herds using newly introduced service sires have suggested that an autosomal dominant gene with incomplete penetrance was involved. Moreover, many umbilical hernias were secondary to umbilical sepsis. Most umbilical hernias were reducible and their size was noticed to increase with coughing. Scrotal hernia is a rare disorder in small ruminants. It forms as an extension of inguinal hernia, when the abdominal organs protrude through enlarged inguinal ring into the scrotum. Unilateral scrotal hernia in male lambs of the Merino, Hampshire, Suffolk and in the Arabic Naimi breeds was described. Scrotal hernia is usually caused by a trauma such as a horn injury in group- housed males.
Conservative treatment:
-
- Trass: a pad on a belt (for supporting hernia).
- Hernial clamp: used to manage reducible hernia less than 5 cm. Two parts of wooden or plastic bars is placed externally to the skin and hernial sac after reducing the hernial content it causes strangulation, necrosis, sloughing of the hernial wall within 10 – 21 days. The scar is subsequently heals by contraction and epithelization.
Surgical treatment:
Indications: 1- When the hernia has not disappear spontaneously.2- In irreducible hernia.
Principle line of treatment:
- Reducing the hernial content,
- Closure of the hernial ring (defect): a- with sutures, b- Occasionally in large hernia, metalic or synthetic fiber mesh prosthesis is used to cover the defect in the abdominal wall.
Technique adopted for abdominal and umbilical hernias:
Positioning of the animal: casting (dorsal recumbency).
Anaesthesia: General anesthesia. Preparation of the animal and site of operation (as usual for abdominal operation).
Procedures:
- Opening of the hernial swelling: by elliptical incision through the skin, fibrous covering of the sac at its center (parallel to the long axis of the body). Isolate the delicate peritoneal covering of the sac.
- Reduce the hernial content intra-abdominally in case of reducible hernia. On the other hand if incarceration due to dissension of the intestinal loop with gas or liquid, may be tapped to diminish the volume or opening the peritoneum and widening the hernial opening. In case of strangulation more care is required in manipulation of the bowel on account of its more or less damaged, but in advanced cases, excision of the part is indicated. In case of adhesion, the peritoneum must be incised to permit of their separation. If not possible to separate, cut the adhesive part round the hernial organ and then reduced together. In case of adhesion, the peritoneum must be incised to permit of their separation. If not possible to separate, cut the adhesive part round the hernial organ and then reduced together. In case of adhesion with omentum, the part may be excised.
- Closure of the hernial ring (defect (Herniorrhaphy). Suture technique used: 1.Overlapping mattress. 2. Modified horizontal mattress. 3. Simple interrupted. 4. Purse string.
Postoperative care:
-
- Abdominal bandage.
- Reduce the amount of food for the first week post operation and gradually returned to normal amount.
- Systemic broad-spectrum antibiotic was given for 3 – 5 days.
- The skin suturing were removed 10 days post-operation.
- Rectovaginal fistula with atresia ani:
It is characterized by the communication between the dorsal wall of the vagina and the ventral portion of the rectum, so that the vulva functions as common opening to the urogenital and gastrointestinal tracts. Usually the abnormality is associated with atresia ani in which the rectum ends as a blind pouch immediately cranial to the imperforated anus.
Surgical management of Atresia ani: A round skin incision was made on the proposed seat of anal opening. The rectal stump was bluntly dissected and identified. The rectal stump was sutured to the skin wound by four interrupted silk stitches at 3, 6, 9 and 12 o’clock direction then the stump was opened at the middle and the collected meconium was squeezed and removed. Simple interrupted sutures were applied between the aforementioned stitches.
Surgical management of atresia ani with recto-vaginal fistula: The treatment was performed by anal reconstruction. A circular skin incision was made at the site corresponding to the anus and flap of skin was removed. The rectal pouch was bluntly dissected and retracted. The blind stump of the rectum was incised and sutured all around with the skin by using interrupted mattress silk sutures. A linear skin incision of 7-8 cm extended horizontally, midway between the anus and vagina was performed. The perineal tissue was separated by blunt dissection then rectal and vaginal walls were separated. The rectal and vaginal wall defects were sutured separately with chromic catgut no.1/0 by Cushing suture pattern. The perineal tissue and skin were closed in standard manner.
- Penile urethral dilatation: is a painless, fluctuating and glistening cystic like pouch covered externally with healthy skin. It varied in size from a small bean like swelling to a large mandarin like size. It extended in front of the scrotum to variable distance on the ventral aspect of the penis.
- Hypospadia: is often accompanied with hypoplasia of the cavernosum urethra. The urethra opens anywhere along its length at one or more locations. Hypospadia is classified based on the location of the urethral opening as glandular, penile, scrotal, perineal, or anal. There has been only one report of hypospadia in goat kids.
- Udder and teat affections: Chronic septic mastitis in small ruminants mainly caused by Staphylococcus spp. Other pathogens such as Streptococcus spp., Enterobacteriaceae, Pseudomonas aeruginosa, Mannheimia haemolytica, Corynebacteria and fungi may contribute in the occurrence of the disease. In addition, severe cases of mastitis related to incorrect preventative strategies have been attributed to the pathogens of Aspergillus fumigatus, Serratia marcescens, P. aeruginosa or Burkholdelia cepacia.
- Chronic purulent mastitis: Stab incision was performed on the lateral aspect of affected half and complete evacuation of the contents was performed. Gangrenous mastitis is caused by virulent strains of organisms producing thrombosis of mammary vessels, infarction and gangrene. Staphylococcus aureus and E. coli with Clostridium welchii produce this condition. Treatment of gangrenous mastitis is performed by mastectomy as usual under the effect of local infiltration analgesia at the base of the udder in a form of ring block using 0.5% lignocaine HCL solution. Supernumerary teats are often seen on the posterior surface of udder and in between the teats. These teats may be functioning or nonfunctioning. It has been reported that, presence of supernumerary teats frequently interferes with free milking process and may predispose to mastitis. Supernumerary teats were removed early in life using curved scissor. In lactating and dry animals, the teats were blocked by 4 and 8% Lotagen® (Byk Gulden Konstanz, Schering-Plough Animal Health, Baulkham Hills, Australia), respectively.
- Udder Amputation: it is indicated in Udder tumors, Udder gangrene. Chronic septic mastitis and when there is a breakdown of the supporting ligaments of a large pendulous udder.
Operation:
- The animal should be controlled in dorsal recumbency.
- In unilateral amputation, the animal is laid on its healthy side with forequarter and head elevated. The fore limbs and the lower hind extremity are fixed to the operation table. The free upper hind limb is held in a fixed and raised position by an assistant.
- The surgical field and surrounding areas are thoroughly cleansed, shaved, disinfected and covered with sterile cloths.
- Make elliptical incisions at the base of the teats.
- The incisions are extended in a straight line in both cranial and caudal directions. Gangrenous and otherwise pathologically altered skin is circumvented. Sufficient skin should be retained to permit the covering of the skin defect excess skin can be trimmed later when sutures are inserted.
- With careful homeostasis, the skin is separated from the udder tissue dorsally with blunt dissection where possible; the first defective is to secure the pudendal vessels in the inguinal region by locating the pulsating A. pudenda externa. Incise the udder fascia, expose the vessels and ligate. Then ligate the perineal vessels and the subcutanea abdominis at the exit from the udder. Dissect the skin from the udder upward to the sulcus intramammaricus and from there dorsally to isolate the diseased half of the udder along the ligamentum suspensorium mamae (medial division) and finally along the abdominal fascia.
- After the isolated udder has been shelled out hemostasis must be checked and completed. Close the wound by means of recurrent single sutures (mattress) of synthetic material.
- Trim away excess skin about 1.5 cm. above the comb of the suture. Infuse the wound cavity with antibiotics or sulfonamides via a teat canula.
- In case of unilateral amputation, affect prophylaxis of the remaining udder half by the intracisternal administration of antibiotics.
- Remove the sutures after eight to 10 day.
10.Eye affections: Pigmentary keratitis, ulcerative keratitis, hyphaema, hypopyon and microphthalmia were among the most common ocular affections recorded in ruminants.
Ulcerative keratitis:
It was treated by flushing of the eyeball with by 2% Boric acid solution. Antibiotic eye drops and antibiotic ointment (Terramycin® (Pfizer) was applied for five successive days. In addition, 1% atropine sulphate solution 3-4 times daily was applied topically to relive the pain as well as intramuscular injection of a broad spectrum antibiotic.
Hyphaema:
Treatment was performed by topical application of 1-2% epinephrine solution for 24 hours only. Then 1% atropine sulphate solution was applied topically to dilate the pupil until all haemorrhage disappeared.
Hypopyon:
Paracentesis and aspiration of the hypopyon by using sterile needle and the anterior chamber is reformed by antibiotic solution.
11.Retention of urine: It means that the animal cannot empty its bladder. This may be partial or complete retention as a result of acute or chronic obstruction of the urine outflow. It may be due to:A) Mechanical causes: as calculi, neoplasms, strictures, prostatic diseases and pressure due to constipation. B) Functional obstruction: This is neurogenic as in cases of atonic bladder, spasms of the bladder neck as in tetanus, colic and painful lesions of the abdomen and pelvis.
12.Urolithiasis:
It means the formation of calculi from less soluble crystalloids of urine as a result of multiple congenital or acquired physiological or pathological processes.
Etiology:
Many factors have been implicated in the etiology of the urinary calculi formation but there are few clinical data supporting any one of them so that urolithiasis is a multifactorial syndrome. In this respect we will discuss some of these factors: I. Dietary errors: 1. Diet of high phosphorus content, 2. Diet rich in silicon, 3. Diet rich in oxalate, 4. Diet rich in calcium, 5. Diet rich in carbohydrates. II. Metabolic disorders: III. Water intake: 1. amount of water: 2. type of water: IV. Urine characters: 1) Urine colloids. 2) Urine volume. 3) Urine pH. V. Infection: VI. Vitamin “A” deficiency: VII. Breeds and hereditary factors: VIII. Sex: IX. Castration: X. Anatomical considerations. XI. Hormones. XII. Stress factors:
Diagnosis:
Uroliths are usually suspected on the basis of typical findings obtained by history and physical examination. When calculi lodge in the urethra, the pressure developed in the bladder will produce mild colic symptoms such as stretching, treading with rear limbs and kicking. The most characteristic sign is an up-and-down pumping of an elevated tail. With trials to urinate, few drops of urine may drip from the perpetual hair.In small animals, urethral pulsation will be easily felt and calculi may be palpated in the urethra. Other signs include: anuria, hematuria and distended or turgid abdomen. Signs of uremia may develop if there are complete obstructive urinary calculi causing symptoms in the following manner, obstruction, irritation, base and injury of tissues. If the blockage persists, either the urethra or the bladder will rupture thus all colic pains and tail pumping will cease. In addition urethral pulsation will disappear. After bladder rupture, the abdomen will take a pear-like form due to the accumulation of urine and inflammatory fluids in the abdominal cavity.
Treatment of obstructive urolithiasis:
Therapy of urolithiasis encompasses the relief of obstruction to urine outflow and elimination of the existing calculi if possible and prevention of recurrence of uroliths.
Medicinal treatment:
The use of specific plain muscle relaxants as aminopromazine HCl. Administration of atropine sulphate sub. /cut. (1 mg for sheep, goat). The use of antispasmodics, sympatholytic drugs (tranquilizer). Usually, such drugs fail even with manual pressure over the urethra.
Surgical treatment:
1) Snip off the urethral process in rams and bucks. To remove calculi lodging in and obstructing the urethra: Animal must be mechanically restrained on its back. By gentle manipulation, the penis is pulled from the prepuce. Snip off the urethral process from its base containing the obstructive calculus.
- Operations for ruptured bladder (Laparotomy)
Indication:
Bladder rupture is a sequel of obstructive urine retention; it requires immediate surgical interference so as to avoid uremia and peritonitis.
Anesthesia and control:
Anterior epidural anesthesia or local infiltration of intended line of incision.
Procedure:
- Prepare the site of operation as usual (paramedian anterior to scrotum).
- Make an incision of about 15 cm. long just anterior to the prepubic tendon.
- Puncture of the abdominal muscles.
- Gradual evacuation of urine from the abdominal cavity.
- By gentle gradual manual traction of the bladder draw it forward toward the abdominal wound.
- Explore the bladder for presence of any calculi, wash it with saline, and introduce a catheter through the bladder to the urethra.
- Suture the bladder rent with double raw of Lembert sutures using 2/0 catgut.
- Flushing the peritoneal cavity with saline solution and put intra-abdominal antibiotics.
- Close the abdominal wound as usual.
- Rumenotomy:
Indication:
It is indicated for removal of ruminal foreign bodies, persistent impaction of the rumen and traumatic reticulitis.
Control:
The operation is performed with the animal in a standing position, either in a stanchion or box stall properly controlled. A kicking strap is applied above the hocks, if considered necessary.
Pre-operative preparation:
- If possible, the entire region of the left flank over the rumen is clipped, shaved and washed with soap and water then dried with sterile towel.
- The skin is disinfected with spirit, then tincture of iodine or Betadine is applied.
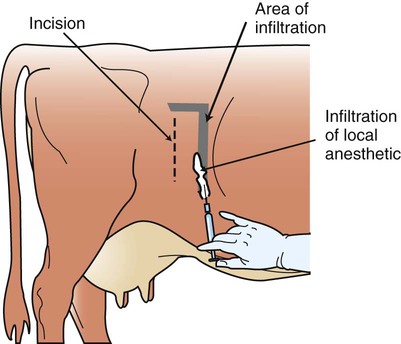
Anesthesia:
- Apply careful disinfection with 70% alcohol or tincture iodine/ Betadine.
- Local anesthesia using inverted – L field block using Xylocaine 2%.
- The horizontal line runs two fingers below the transverse lumbar processes and the vertical line runs behind the last rib by 2 fingers breadth and 10 cm downwards. The anaesthetic is injected under the skin, in the muscles and on the peritoneum.
- The animal must be given Xylazine2% I/M at a dose of 0.15 mg/kg body weight.
Operative technique:
Weingart`s Technique:
- An incision of about 7 – 10 cm in length is made through the skin (a few inches posterior to and parallel with the last rib at a distance of 2 fingers below the transverse processes of the lumbar vertebrae).
- The incision is continued through the external and internal oblique as well as transversalis muscles thus exposing the peritoneum.
- Hemorrhage is controlled.
- The peritoneum is then carefully incised exposing the rumen, a portion of the rumen is pulled through the incision and maintained in position to the bow by means of two special forceps.
- The ruminal wall is then incised between the two forceps and an incision of about 15 – 18 cm in length continued upwards and downwards.
- The margins of the rumenal incision are then stretched to the bow by means of a series of special hooks, 3 or 4 on each side.
- The hand is introduced to the rumen, then the reticulum and search for the foreign bodies is made.
- The reticulum should now be explored thoroughly for foreign bodies and for adhesions to the diaphragm or floor of the abdomen.
- In palpating or removing penetrating objects one should carefully avoid breaking down any existing adhesions which might be successfully preventing the spread of infection.
- The ruminal incision is then closed with two rows of continuous Lembert sutures, using catgut no. 0.- The first stitch of the row is made in a transverse direction at the lowest point of incision, 1/2 inch of the rumen wall is turned in, tied and the two serious surfaces brought together.
- The needle is then inserted close to the knot and advanced up. As the top is reached, the stitching is made downwards in a diagonal way and this confirms the first row of sutures.
- The exposed portion of the rumen is then swabbed and is powered with penicillin streptomycin, then the bow and forceps are removed and the rumen is replaced into the abdomen.
- The peritoneum and transversalis muscle are taken together in the first line of continuous abdominal sutures. Care is always taken to make sure of an air tight closure. A dose of aqueous penicillin streptomycin is injected into the abdominal cavity before the complete closure of the peritoneum.
- The internal and external oblique muscles and the fascial layers are included in the next row of sutures. The skin wound is closed with silk. Usually the stitches are removed 10 days later.
- Intestinal prolapse:
The condition was corrected by flushing of the prolapsed part of intestine with sterile normal saline solution and reduction of the prolapsed part inside the abdominal cavity. The abdominal opening was closed with interrupted mattress silk sutures.
- Congenital anomalies:
- Arthrogryposis is common in ovine.
- Contracted flexor tendons and arthrogryposis are caused by autosomal recessive gene and it is the most prevalent abnormality in the new born calves.
- Congenital intestinal prolapse through the persistent umbilical opening in the new born kid has been reported earlier.
- Hypothermia, Hyperthermia, and Sunburn:
Newborn lambs and kids and recently shorn sheep and goats are susceptible to hypothermia, hyperthermia, and sunburn. Frequency of neonatal observations should be increased, and appropriate shelter should be provided if natural conditions do not offer sufficient protection.
- Tail-Docking: Tail-docking of lambs is performed to reduce the possibility of soiling the long tail with urine and feces and the subsequent development of fly strike, a potentially fatal condition. With hair-breeds of sheep, tail-docking may not be necessary. Goat kids have an erect tail that is not docked. Tail-docking of wool-breed lambs is recommended unless the life span is limited to a season when fly infestations are unlikely and when the feed used does not result in a heavily contaminated fleece. There are several acceptable methods for tail-docking. These include rubber rings, hot-iron cautery, surgical removal, and surgical removal after application of an emasculator, and various combinations of the basic procedures. Tails should be docked when lambs are as young as possible, preferably before 2 weeks of age. Very short tail docking should not be permitted because it increases the incidence of rectal, and perhaps vaginal, prolapses.
- Castration: Rams and bucks are castrated to prevent indiscriminate breeding and fighting, thus exercising genetic control, regulating the time of year of lambing, controlling the minimum age of first parturition and lactation, and reducing injuries. There are 3 commonly accepted methods for castrating rams and bucks: application of rubber rings, crushing the spermatic cord with an emasculator (i.e., the Burdizzo method), and surgical removal of the testicles; various combinations of the three are also common. For each method, the lamb’s or kid’s scrotum should be palpated to make sure that it contains 2 testicles and that there is no evidence of an inguinal hernia. The castration procedure should remove both testicles unless an approved experimental method precludes bilateral castration. A common recommendation is to castrate lambs and kids when they are between 24 hour and 7 day of age, although recommendations vary. Tetanus prophylaxis is indicated. For very young goats, castration is similar to calf castration. The distal one third of the scrotum is removed with a scalpel. Each testicle is stripped from the scrotal fascia and pulled ventrally to tear the spermatic cord. The incision is left open to drain and heal by second intention. For older animals, either heavy sedation or general anesthesia in combinations with local anesthesia is indicated. The distal one third of the scrotum is removed with a scalpel. Each testicle is stripped from the scrotal fascia and cremaster muscle to expose the spermatic cord. A transfixation ligature is placed in the spermatic cord. An emasculator is placed on the spermatic cord distal to the ligature to provide hemostasis and remove the testicle. The incision is left open to drain and heal by second intention.
- Disbudding and Dehorning: Disbudding of goats should be performed at less than 1 month of age for ease of the procedure and effectiveness of removing all of the horn bud. Cautery with heat should be used when possible and be considered the method of first choice, although surgery, freezing, and an acidic paste are other options. Horns of adult goats and calves should be removed under general anesthesia or sedation and local anesthesia due to the anatomy and tissues involved and the significant development of horny tissue in older goats, especially bucks. Following sedation and cornual nerve block as describe above, an incision is made with a #15 scalpel blade around the base of the horn. The scalpel is then be used to cut under the horn bud to remove it. Pressure is applied for hemostasis. The site will heal by second intention. Alternatively, a portable dehorning iron can be used.
- Caesarean section (C-Section): C-section is indicated when rolling is unlikely to succeed to correct uterine torsion and variety of genital conditions associated with dystocia (difficult parturition). A c-section is a relatively easy and quick procedure. I prefer to have the females heavily sedated, positioned at 45° angle between sternal and lateral, leaning towards the right to expose the left flank. A ventral midline procedure can be performed, but in my opinion this stresses the goats more and may compromise breathing. If careful, all the lambs/kids can be removed through an incision in one horn.
- Neoplasm: Although several cases of skin neoplasms were recorded in sheep and goats. Tumours or neoplasms may be defined as” an abnormal mass of tissue, the growth of which extends uncontrolled in compensation to the normal tissue and persists in the same excess even after cessation of the stimuli which evoked the change”. Tumours are that can be observed anywhere over the body of the animal.
Diagnosis: History and clinical signs/ examination: location, size and consistency. Histopathologic (biopsy) examination (exploratory cytology) to confirm the diagnosis and to determine the nature of the tumour. Radiography: bones and vascular organs.
Treatment: General line of treatment: Definitive excision-refers to the use of surgery as the sole treatment procedure without adjunctive radiotherapy or chemotherapy. Local excision: the removal of a neoplastic mass with the minimal amount of the surrounding normal tissue. Wide local excision: removal of a significant predetermined margin of surrounding tissues together with the primary mass. Radical local excision: removal of a tumour with anatomically extensive margin of tissue e.g., sacrcoma. Apart from surgery and chemotherapy radiation, cryosurgery (freezing), hyperthermia (heating), or immunotherapy can be effectively used to treat. Radiotherapy: The aim of use of this method is the destruction of malignant cells by gamma radiation. Anyway this technique is better to be used in adjunction with surgical de-bulking. Cryotherapy: It depends up on two cycles of freezing and thawing.
References:
Abd El Hady AAA 1993. Studies on the prevalent surgical udder and teat affections in dairy farms. MVSc, Cairo University.
Ansari MM 2014. Fundamentals of General Veterinary Surgery (A book for both undergraduate and postgraduate level). First edition, Published by Satish Serial Publishing House, Delhi-110033 (India). ISBN 978-93-81226-00-0.
Chauhan HVS 1997. A Text Book of Veterinary General Pathology: 1st ed, International Book Distributing Company, Lucknow, pp: 156-157.
Senna NA and Abu-Seida AM 2004. Clinical and surgical aspects of certain congenital anomalies in cattle and buffaloes. Vet Med J Giza, 52: 347-362.
Senna NA, Abu-Seida AM, Gadallah SM, El-Husseiny IN and Rakha GM 2003. Congenital anomalies in native breeds of sheep and goats: A report on 120 cases of 24 varieties. Vet Med J, 51: 363-380.
Smith BP 1983. Diseases of the alimentary tract. In Large Animal Internal Medicine. 2nd edn. Philadelphia, Mosby. pp 858-860.
Valentine BA 2004. Neoplasia. In: Farm Animal Surgery. (Fubini SL, Ducharme NG, Eds.), Saunders. An Imprint of Elsevier, USA, pp.23-44.
*****