PREVENTION & CONTROL OF UROLITHIASIS (STONE) IN ANIMALS
Obstructive urolithiasis is the retention of urine subsequent to lodgment of calculi anywhere in the urinary conduct from up to urethral orifice. The disease results in heavy economic losses to the livestock industry as it is attributed the fifth most prevalent cause of death in feedlot. Obstructive urolithiasis is a serious, potentially fatal condition, most commonly causing symptoms in castrated male animals, but also occurring in breeding males. Nutritional management is the best preventive strategy against urolithiasis. As such it may not replace the surgical procedures but may surely help in decreasing the recurrence rate of uroliths. Urolithiasis is a common problem in both ruminants and non-ruminants and nutrition plays a significant role in predisposing urolithiasis. The nutritional factors mainly influence urinary constituents and pH, which affect stone nucleation and growth. While surgery can render a patient stone-free, non-operative treatment modalities are required to prevent and reduce the risk of recurrent urolithiasis. Moreover, long-term pharmacological therapy and its potential side effects often lead to subsequent failure. In this regard, nutritional management is the best preventive strategy against urolithiasis
Introduction
Urinary system is designed to dispose of body wastes in liquid form and the normal urine is in a state of meta-stable over-saturation (i.e. no spontaneous precipitation). The urine is a complex solution that allows mineral salts to be kept dissolved under over- saturation conditions. The urolithiasis presents a state of unstable over-saturation where a spontaneous precipitation exists and minerals precipitate, the crystals do not dissolve and they add together allowing the growth of the urolith (also called ‘urinary stones’ or ‘calculi’).
It is a condition of the urinary tract in which insoluble mineral and salt concretions develop and aggregate around a nidus of proteinaceous material mainly within the bladder or urethra but it can occur anywhere in the urinary tract. Abnormal microscopic precipitates in urine are known as crystalluria whereas macroscopic concretions are called uroliths.
Types of Stone
There are mainly 5 types of stones – struvite calcium oxalate, calcium phosphate, calcium carbonate and silica. Uric acid, cystine, hippuric acid,and tyrosine crystals may also be found. The presence of a specific type of crystal depends on the diet and transitory physical and chemical conditions that exist in the urine at that time
Incidence
1) Species – Goats are most commonly affected followed by cattle, cats and dogs.
2) Age – In ruminants, young animals below 6 months of age are more affected because of high protein diet. Canines of middle age group (3-7yrs) have the highest incidence of urolithiasis.
3) Sex – Urolithiasis is not generally found in females due to flexible lumen of urethra.
4) Urinary pH – Acid pH of urine leads to precipitation of uric acid and cystine uroliths. Similarly, alkaline pH of urine leads to precipitation of struvite, calcium carbonate and calcium phosphate uroliths. However, solubility of silicates and oxalate uroliths don’t depend on urinary pH.
5) Castration status – Castrated animals are more susceptible than un-castrated ones.
6) Season – There is highest incidence of urolithiasis in ruminants during months of extreme winter (December-February) and extreme summer (March-June). However, the trend is reverse in canines where least number of cases is recorded during months of January and February.
7) Dietary habit – Obesity and associated dietary
Etiology
The etiology is complex and multifactorial. Although urolithiasis is known to have numerous predisposing etiology factors , but exact mechanism of stone formation and growth is not fully known. Urinary calculi formation usually results from a combination of various physiological, nutritional and management factors. It may occur due to excessive or imbalanced intake of minerals in feedlots while fattening cattle receive rations high in cereal grain and oil meals. These feedstuffs have high levels of phosphorous and magnesium but relatively low level of calcium and potassium predispose to disease condition A calcium phosphorous imbalance results in high urinary phosphate excretion which is an important factor in the genesis of phosphate calculi . Numerous additional factors have been incriminated as contributing causes of the development of phosphate
calculi with resultant obstructive urolithiasis in cattle.
These include heavy concentrate-low roughage diets, limited intake or deprived of water, dehydration, urine alkalinity, mineralized artesian water, alkaline water supplies, excess of sodium bicarbonate in diet, vitamin imbalance e.g hypovitaminosis and hypervitaminosis
and high protein rations . Less frequently uroliths composed of silica, carbonates or oxalate. Livestock grazing in pastures containing large quantities of oxalates, estrogen or silica are prone to develop these types of calculi. Urolithiasis in castrated beef cattle has been reported to be associated with diethylstil- bestrol implants . Geographical and seasonal influences play an important role for range herds in semi-arid areas. In addition, the anatomy of the male ruminant urinary tract also contributes due to the potential narrowness of the passage and tortuous route.
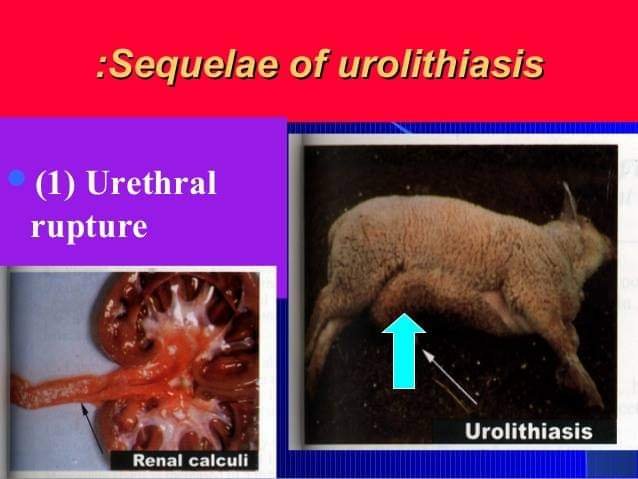
The sigmoid flexure is a common site for uroliths to lodge in all ruminant species . Uroliths may also be fount on lesser occasion at the ischial arch. In small ruminants the urethral process is an extremely common site for uroliths to lodge .
Clinical signs
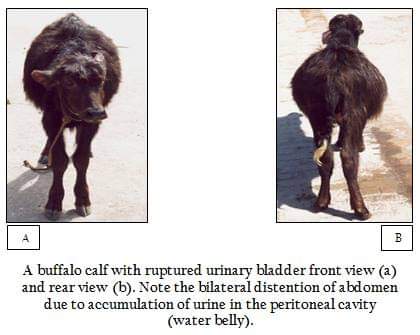
The clinical signs associated with urolithiasis depend upon the degree of obstruction to free flow of urine. Severity of surrounding tissue reactions .
The major clinical signs reported during the onset of urolithiasis include anorexia, suspended rumination and decreased water intake. Animals suffering from partial obstruction dribble blood tinged urine after prolonged, painful attempts of urination, as the disease progress, the symptoms depicted are abdominal bilateral distention, tenesmus, colic, and weight shifting, and grinding of teeth, urethral pulsation and tendency of rectal prolapsed. Animals may have an arched stance, tread their feet, swish the tail, or kick at their belly. Urolithiasis should always be near the top of the differential list in male ruminants with signs of colic, particularly in sheep and goats. Stranguria, anuria, oliguria, hematuria, mineral deposits on the urethral hairs, uremic odor to the breath, urinary
bladder distention and pulsations of the pelvic urethra may also be present. Less specific signs include rectal prolapse, rumen stasis, tachycardia and tachypnea.
There is severe damage to the bladder and urethral mucosa by uroliths which leads to haematuria , oligouria and dysuria . In terminal stages, the temperature start decreasing, due to retention of metabolic wastes and their reabsorption results in toxaemia . Complete urethral obstruction results in death due to uraemia
Treatment
Surgical intervention is the primary step to release the pressure from bladder, which is further treated by medicinal means to establish the animal towards normalcy.
Various treatment modalities, both medical and surgical for the management of urolithiasis have been developed in almost all the species . In ruminants, obstructive urolithiasis can be successfully treated if recognized early in the clinical course . In mild cases, the animals can be treated by using tranquilizers and antispasmodics , litholytic drugs like cystone. Diuresis should not be used before the removal of calculi and afterwards their administration is generally not required. Since there is hyperkalemia, hyponatremia and hypocalcaemia, therefore stabilization of such metabolic derangements often involves
administration of intravenous fluids for several hours,with repeated assessment of hydration, acid-base balance and serum electrolyte concentrations. Such treatments occasionally involve concerns about exacerbation of bladder distention in animals with an intact bladder. The animals that shows raised levels of BUN and creatinine can be effectively treated by peritoneal dialysis .The treatment of obstructive urolithiasis is
primarily surgical . Recurrent urolithiasis, calculi at multiple sites, badly damaged urethra, atonic bladder or severe cystitis leads to failure of surgical repair in obstructive urolthiasis . Urethrotomy, either post scrotal or post-ischial at the site of calculi lodgement is widely recommended and practiced to relieve the obstruction . However, postoperative leakage of
urine from the site of obstruction leads to necrosis of urethra and subcutaneous tissues. Further, postoperative urethral constriction and recurrent urolithiasis are potential factors that results in the unfavorable outcome after urethrotomy, . Other surgical methods include penile catheterization cystotomy and bladder fistulation , intra pelvic cystic catheterization and peile amputation and, tube cystotomy is in voyage. The technique of tube cystotomy is a method of fixation of tube in the urinary bladder for the free passage of urine, followed by chemical dissolution of calculi which shows excellent results. Cystotomy tubes provide a practical method for the urinary diversion when more radical surgical procedures are not feasible . Cystotomy tubes bypass urinary outflow obstructions or as an alternative to the urethral catheterization . Several different types of tubes are available, including Foleys catheters, Mushroom tip catheters and percutaneous catheters; more recently low profile gastrostomy tubes have been adapted for the use in cystotomy tubes . Cystotomy
tubes should remain in place for at least 14 days before removal to ensure adequate adhesions between the bladder and the body wall to reduce the possibility of
urine leakage or peritonitis . Tube cystotomy is not free from complications and some complications involved are urine leakage, wound infection or dehiscence problems with the tube itself such as irritation at the stoma site, obstruction or accidental dislodgment and problems related to ascending infection due to the presence of the tube
Limitation of Surgical Treatment:
Various limitations of surgical therapy are difficulty in detection of urolithiasis at early stage, costly, quite common recurrence, careful follow up for a number of years, risks to long term fertility, potential side effects and no guarantee
Preventive measures in Ruminants
Composition of uroliths together with environ-
mental and dietary factors should be considered when establishing adequate preventive measures for urolithiasis . Critical preventive measures such as providing calcium to phosphorous ratio of 2:1 in the complete ration, increasing the salt levels to 4 percent of the diet in order to stimulate water consumption and to increase urine volume and maintenance of adequate and abundant water supplies should be highly considered
. Struvite crystals can be prevented by the dietary modification to induce urine acidification . The ration should be modified, which includes elimination of alfa-alfa feeding, reduction or elimination of grain feeding,a change to grass hay as primary forage, encouragement of grazing and ammonium chloride supplementation. These modifications are intended to reduce the urinary load of calculogenic minerals, especially calcium and phosphorous through elimination of alfa-alfa and grain feeding respectively. Besides potentially altering the mineral content of the diet, free access to grazing may increase the daily amount of water intake, which may in turn dilute urine, thus limiting calculo-genesis. Changing from legume to grass hay and feeding ammonium chloride may move the dietary balance of
strong cations and anions towards greater concentration of strong anions. Those areas where sheep exclusively are fed on paddy grasses in winters due to non availability of pastures, fortifi-cation of the dry paddy grass need to be undertaken to reduce the oxalate content of the grass . Provision of clean water in multiple sites and intentional salting moistened grass hay, induction of diuresis and maintenance of dilute urine would help a long way keeping urolithiasis in check . Screening of the animals be treated mandatory to categorize them as stone formers and non-stone formers before the disease is manifested clinically.
General Preventive Strategies
- Optimize use of high quality forage – Ruminants need a minimum of 1.5% of their body weight as forage to ensure a healthy rumen
- Strategic use of concentrate feeds;
- Optimum level of Ca: P (1:1 to 2:1) to avoid precipitation of excess phosphorus in the urine;
- Ad libitum feeding to avoid marked changes in urine concentration;
- Free choice of water; [The susceptibility of calves to urolithiasis increases when the water intake per unit forage DM intake declined below 3.5.]
- Supplemental feeding of NaCl @ 3.5% of daily DM intake to promote greater water intake;
- Strategic supplementation of calculogenic feeds like cottonseed meal, sorghum, Bengal gram, cotton seed meal, clovers, triticale and oxalate containing plants and feed supplements like stilbestrol, diethylstilbestrol, lime stone and sugarcane bagasse.
- Grazing management practices like
a) Allowing only females to graze the risky pastures;
b) Permitting limited access of wethers and steers to oxalate rich pasture;
Specific Preventive Strategies
1) Calcic uroliths (Calcium oxalate and Calcium carbonate):
- Low calcium, Low oxalate and High moisture .Restrict animal protein, vitamin C and NaCl, Do not restrict phosphorus and magnesium .Supplement Vitamin B6 and potassium citrate (100-150 mg/kg/day) to prevent recurrent Ca-oxalate stones
- Low arachidonic acid
- Low feeding of pelleted alfalfa to decrease the incidence of calcium carbonate stones
- Higher dose of citrate inhibits calcium absorption; phytic acid and/or zinc may also be useful for treatment
2) Phosphatic uroliths (Struvite, Calcium
phosphate) Maintenance of a total ration Ca: P of 2:1 and a dietary Mg level at 0.2-0.3% (DM basis) will prevent phosphatic urolithiasis. Majority of ammonium and phosphate in urine comes from protein in diet. So, low protein diet should be fed. The uroliths can be dissolved effectively by various acidifiers like 4% NaCl, 10% acetic acid, D, L methionine, ascorbic acid, 0.5-1% NH4Cl ( or 45g/day to steers and 10g/day to sheep) and phosphoric acid. 3) Siliceous uroliths - Supplements containing 3-5% NaCl or 1-2% NH4Cl
- Phosphorus supplementation
- Avoid high plant proteins (e.g. soybean hulls, corn gluten)
- Water intake >200 g/kg b.w./day
Cystine uroliths: Potassium citrate, sodium bicarbonate, CaCO3 and lactate can be used.
Preventive measures in Pets In dogs and cats, struvite urolithasis is most common followed by urate, cystine, and calcium oxalateGeneral Preventive Strategies
- Low level of high quality protein to reduce excretion of urea;
- Low calcium, phosphorus and magnesium to reduce concentration of calculi constituents;
- High sodium to induce a large volume of low concentration urine;
- Typical diet for treatment of urolithiasis in dog should contain 8% protein, 0.3% calcium, 0.12% phosphorus, 0.02% magnesium and 1.2% sodium in the DM, 1-2 mg/kg/day K, 1-2 mg/kg/day Zn and 100-
200 mg/d Vit. B12.
Specific Preventive Strategies
1) Struvite uroliths: Diets should have a low content of magnesium and phosphorus. Urine pH should be lowered and output increased by feeding low protein, high sodium diet. Water consumption of pets can be increased by switching pets from dry food (<12% water) to wet food (75% water). When feeding of wet food is not practical, dry food is supplemented
with urinary acidifiers like NH4Cl salt (0.5-1% of DMI) or 1-2g D, L-methionine. NH4Cl is unpalatable. So, table sugar can be added in diet. Molasses should be avoided as flavoring additive because its high potassium content may diminish the acidifying effect of NH4Cl.
2) Urate uroliths: It is treated by feeding diets containing around 10% protein and 70% moisture in dogs.
3) Cystine uroliths: It is treated by feeding low protein and low sodium diets. Commercial calculo- lytic diets for all types of uroliths are prescribed by Hill’s Pet Nutrition, U.K.
TREATMENT-—
Following line of treatment has been done by me at the field level on more than 50 male goats n calf, and has got marvelous result in some cases with 100% result.
Allopurinol (Zyloric®) was administered @ 10 mg/kg of body weight per os, bid for 3 days, along with Ketoprofen @ 3 mg/kg of body weight I/M, sid. The animal started urination 3 hours after the first dose of medication and completely recovered after treatment of 3 days.Apart from this we can also give-
Herbal Products with Antiurolithiatic Activity: The marketed composite herbal formulations, Cystone (Himalaya Drug Company, India), Calcuri (Charak Pharmaceuticals, Bombay, India) and Chandraprabha bati (Baidyanath, India) have been widely used clinically to dissolve urinary calculi in the kidney and urinary bladder
HOMEOPATHIC TREATMENT-—
Cantharis—200
It is given 10 drops thrice a day to goat/calves for 15 days orally.
By
Dr Ajeet Kumar Singh
Veterinary Surgeon
Founder and director of Global Veterinary Clinic and Surgery Centre Gorakhpur
Reference-On request.