USE OF LASER THERAPY : A NEW PARADIGM IN VETERINARY PRACTICE
Compiled & Edited by-Dr. Charulata, PhD,Pantnagar
Veterinary laser therapy is an innovative treatment that has gained popularity in recent years as veterinarians discover its benefits for pets. Used similarly to acupuncture, massage therapy, and other alternative therapies, laser treatment can be used in conjunction with or in place of medication to manage pain, inflammation, and wound healing.
Laser therapy is a novel rehabilitation technique being used in veterinary medicine for both rehabilitation and therapeutic purposes. Photobiomodulation (PBM) induced by laser therapy is the application of electromagnetic radiation within the near infrared spectrum and is aimed at stimulating healing or analgesia within the target tissue. Currently laser therapy is being advocated for a variety of conditions some of which include musculoskeletal pain, osteoarthritis, joint pain, and inflammation, neuropathic pain, otitis, dermatitis, chronic, or non-healing wounds and decubital ulcers .
There are three phases of wound healing; the inflammatory, proliferative and remodeling phases. The inflammatory phase is initiated at the time of injury and begins with hemostasis and formation of the platelet plug. Platelets release platelet-derived growth factor which attract neutrophils and more importantly macrophages. Macrophages attract fibroblasts and therefore commence the proliferative phase. Fibroblasts differentiate into myofibroblasts and cause tissue contraction. Tensile strength is increased by collagen reorganization and the eventual outcome is a wound that reaches 80% of the strength of uninjured tissue . It has been shown in experimental studies that laser therapy reduces pain, positively influences inflammatory, proliferative, and maturation phases of wound healing and increases wound tensile strength . However, most of these studies have been in laboratory animals and do not account for the difference in wound healing between species.
“Laser”—an acronym for “light amplification of stimulated emission of radiation”—refers to a unit that emits focused, penetrating light beams in three forms:
- Monochromatic:Light that is a single wavelength (as opposed to natural light, which is emitted as a range of wavelengths)
- Coherent:Photons (i.e., tiny particles of light or electromagnetic radiation) that travel in the same phase and direction
- Collimated:Photons that travel in a single straight beam
Coherence and collimation give a laser penetrating power to a restricted area so that nearby tissues are unaffected.
Lasers are classified based on their wavelength and potential energy output, with four classes currently recognized:
- Class 1lasers, such as barcode scanners used in supermarkets, are used safely every day
- Class 2lasers, which include laser pointers and some therapeutic lasers, produce a beam in the visible spectrum (400–700 nanometers)
- Class 3lasers include the most commonly used therapeutic lasers
- Class 4lasers cause thermal injury to tissues and include surgical lasers used to cut and cauterize tissue during surgical procedures
How does laser therapy affect my pet’s tissue?
Therapeutic lasers use light waves of a specific wavelength to cause photobiomodulation, or the alteration of cellular and tissue physiology. Light absorbed by cellular components stimulates electrons and activates cells to promote growth, proliferation, migration, and repair.
The type and depth of tissue that responds to laser therapy depends on the wavelength of the light that is delivered. Most therapeutic lasers use red or near-infrared light, which has a wavelength of 600–1070 nanometers, although units with green, blue, and violet light, which have lower wavelengths, are becoming more popular. Laser beams of lower wavelengths are absorbed by superficial tissue, such as the skin, whereas beams of higher wavelengths penetrate deeper to muscles and bones.
Laser therapy helps tissue repair by causing the following:
- Endorphin release
- Vasodilation, which increases blood flow to bring in oxygen and cells involved in the healing process
- Muscle relaxation
- Decreased inflammation
- Faster healing and repair
The main clinical benefits of laser use in pets include decreased inflammation, decreased pain, and improved wound healing.
Who can benefit from laser therapy?
Laser therapy is used for many veterinary medical conditions, including:
- Chronic arthritis
- Surgical incisions
- Tendon and ligament injuries
- Traumatic injuries
Laser therapy is particularly useful for pets with limited medical treatment options, such as:
- Pets with liver disease who cannot take medications
- Cats, for whom only a few pain-control medications are approved
- Exotic pets for whom medication administration is difficult or impossible
- Older pets with diminished organ function
How are laser treatments administered?
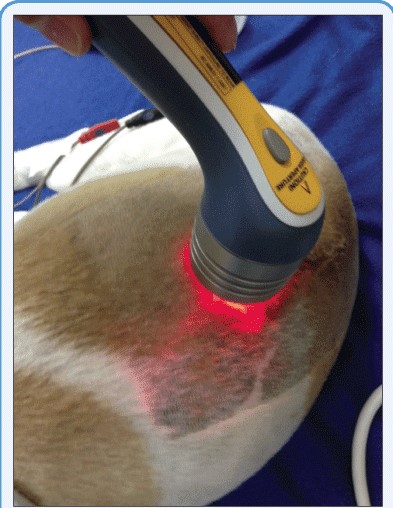
During a treatment session, the handheld laser wand is slowly moved back and forth over the damaged tissue, producing a warm, pleasant sensation that most pets seem to enjoy and find relaxing. Sessions usually last 15 to 30 minutes, with the number of sessions and frequency of treatments dependent on the injury. Chronic conditions may be treated weekly, whereas surgical incisions and open wounds often require daily treatment.
Is laser therapy safe for pets?
Laser therapy is safe if performed correctly, using the proper settings and treatment durations. Higher-powered units can cause thermal burns to tissues if used incorrectly. Also, laser beams directed at an eye can cause permanent retinal damage, so patients and all veterinary staff must wear protective goggles during treatment.
PRINCIPLE OF LASER THERAPY
Laser therapy has three broad effects on animal tissue: it decreases inflammation, decreases pain, and it accelerates healing. These effects of near-infrared laser light in tissue are best described through Photobiomodulation since some parts of the healing process are accelerated (organization and proliferation), while other parts are diminished (inflammation). The initial effect of near-infrared laser light is the stimulation of the production of adenosine triphosphate (ATP), reactive oxygen species (ROS), and nitric oxide (NO) .
In turn, these bioactive substances cause the cascade of effects for each of the three mechanisms of action involving inflammation, pain, and healing . Further, these effects are not the result of heating or warming the tissue (photothermal). Instead, they are the result of a photo biochemical change skin to the events that occur with photosynthesis or vitamin D synthesis: biological changes in chemistry at the cellular level, caused by the light .
THERAPEUTIC DOSING
Formulation of the appropriate therapeutic dosing of laser therapy needs understanding the dose-dependent nature of tissue response to infrared light. Similar to dosing tissue with antibiotics (mg/kg) or radiation (J/kg = Gy), tissue must receive the appropriate target dose of light energy to manifest the effects of laser therapy. However, for laser therapy, the dosing is in joules per square centimeter (J/cm2). If suboptimal doses are administered, then the effects will also be sub-optimal, or may even not be apparent. Multiple current publications indicate that proper dosing for most superficial tissue is in the 1-4 J/cm2 range while dosing for most deep tissue is in the 8-20 J/cm2 range [7,20].
To facilitate delivering proper doses of laser therapy, power, wavelength, and pulsing must be understood . Doses are affected by tissue type, anatomic site, tissue depth, species, coat color and length, skin color, and body condition score . Effective dosing intervals (again, just like with antibiotics or radiation therapy) are critical to achieving positive clinical outcomes. Factors such as patient preparation, application techniques, frequency of administration, and proper patient management are also essential for optimal results .
Laser basic
Laser light has a specific property that helps to distinguish it from other light sources (sunlight) and it consists of a monochromatic, coherent, collimated light. Monochromatic is essentially when light is emitted from the unit, it is a single wavelength, unlike natural light, which is emitted at varying wavelengths. This property allows the production of light targeted for absorption by a specific tissue and specific use .
Depending on the unit, several wavelength options may be available for different therapeutic uses. Coherence is characterized by photons that emerge from the unit and travel in the same phase and direction. Collimation describes light that is emitted from the unit and does not diverge. Coherence and collimation allow the laser to penetrate the skin, treating only a small area of the body, while minimizing/avoiding unwanted effects to other tissues, such as heating and/or damaging the skin .
Laser light is monochromatic (one wavelength), coherent (all photons travel in the same phase and direction), and collimated (minimal divergence of the laser beam over a distance). These three properties allow the therapy laser light to be focused on a specific area of the body, to penetrate the skin without heating or damaging it, and to interact with tissue with few side effects. The beam should be aimed at 90° to the surface of the area being treated. Wavelength influences the depth of penetration, and longer wavelengths penetrate deeper into the tissues. The optimal wavelength range for tissue Photobiomodulation appears to be 650nm to 1,300nm; at longer wavelengths, the laser beam penetrates deeper into tissue while minimizing absorption by the pet’s hair and skin pigment. Superficial wounds and joint injuries can be treated with shorter wavelengths, while longer wavelengths are better suited to treat muscle injuries .
Tissues interact with lasers in varying ways, allowing light to be reflected, scattered, transmitted, or absorbed. Reflection of photons takes place at the epidermis; reflected photons not only lack clinical effect but can also be responsible for tissue damage (e.g. to the eyes and gonads). Scattering occurs once the photons penetrate the tissue. Each time the scattered photons strike an object outside the target tissue, the amount of photon energy is reduced. Transmitted photons also lack clinical effect because they pass through the tissue without being absorbed. The absorption of photons by the target tissue realizes the therapeutic benefit of lasers .
Photobiomodulation is a photochemical process in which photons from a laser source interact with the target cells via a non-thermal mechanism to cause either stimulation (upregulated) or inhibition (downregulated) of biochemical pathways. These lights are absorbed as photons (bundle of light) . A chromophore is responsible for a molecule’s color and, in biologic molecules, undergoes a conformational change when hit by light, such as a laser. This change in the chromophore excites cells and can alter, or speed up, cellular reactions. Commonly noted chromophores include hemoglobin, water, melanin, proteins, and amino acids. The thought process is that these compounds when exposed to laser light-cause alteration of cellular functions, allowing increased healing and/or recruitment of secondary mediators to facilitate healing .
Cytochrome C which is located in the mitochondria serves as an important photoreceptor. When laser light is absorbed by a chromophore or cytochrome C, a biochemical change can occur that is mitochondrial respiration and ATP production increase, leading to global tissue effects. Besides, low-level laser therapy, low light therapy, or non-ablative laser therapy, and cold laser therapy (however, heat is produced during clinical treatments), have also been used and this treatment differs from more invasive laser surgical procedures. Several in vitro studies have been performed on light’s effects on various types of cells such as increases in angiogenesis, neurite extension, normalization of ion channels, stabilization of the cellular membrane, and a host of other cellular changes have been investigated .
Power
Power is a unit of time and is expressed in watts (W) or milliwatts (mW). One watt is one Joule of energy delivered per second, and the laser dose is typically expressed as Joules/cm2-the energy delivered over a surface area. The power of the therapeutic laser matters in terms of the dose delivered, and the time needed to deliver the treatment dose. The power density or intensity indicates the amount of power in a given surface area, while the spot size of the laser indicates the surface area size that can be treated when the laser is held stationary .
Lasers with larger spot areas have a more homogeneous passage of the photons with less scatter. The energy of the laser characterizes the power emitted over time, measured in joules. Frequently, energy density is used to report the dosage of the laser in joules per cm2 (J/cm2). The most commonly used therapeutic lasers in veterinary medicine are Class III lasers, which may deliver energy from 1mw to 500mw, and Class IV lasers, which deliver power at greater than 500mw .
Wavelength
Laser light wavelength and frequency determine the way the laser light interacts with its target tissue . Wavelengths are typically measured in nanometers (nm). Wavelength is important when determining the biological effect of lasers on tissues. Tissues, such as melanin and proteins, absorb ultraviolet light (100-400 nm). Light on the other end of the spectrum (1400-10,000 nm) is absorbed by water. Therefore, optimum wavelength ranges of 600 to 1200 nm which minimize scatter and maximize absorption are recommended for tissue penetration .
A lower watt laser provides less energy delivery to deeper tissues so the time needed to deliver treatment is longer. A lower power laser is better suited for treating superficial structures because of the limited power density to drive photons into the deeper tissues. A higher watt laser allows the treatment to be delivered over a shorter period and involves administering the laser energy with a sweeping motion over the affected area. This sweeping motion may provide more complete coverage of the treatment area and may cover surrounding areas that could be causing secondary or referred pain. Pulsing of the laser beam may provide less heating of tissues at the surface while allowing for an adequate level of energy to reach the deeper target tissues, but more research is needed to define the optimal approach to a pulsed laser beam .
The carbon dioxide (CO2) laser emits a coherent, collimated, and monochromatic beam of light at a wavelength of 10600 nm. Wavelengths of laser light are highly absorbed by water followed by hemoglobin, melanin, and some proteins resulting in photothermal laser-tissue interaction. A high degree of absorption of CO2 laser light by water allows precise cutting of tissue via vaporization of the intra- and extracellular fluid and destruction of the cell membranes. The CO2 laser can seal and coagulate small blood vessels (up to 0.5 mm), lymphatics, and nerve endings resulting in better visualization. Non-contact mode of excision with laser can reduce intraoperative wound contamination by tumor cells .
Continuous or pulsed emission of photons
Photons can be emitted either continuously or by pulse. Continuous emission implies that radiation is emitted at constant power for the entire duration of use. Pulsed therapy implies that radiation is delivered in cycles over the entire duration of use, with time spent one of 2 ways: radiation emitted or no radiation emitted. Currently, there is a debate for the superiority of continuous versus pulsed therapy. Some have suggested that there is no difference, while others have shown that pulsed therapy may be more effective .
Laser classification
Laser classification is based on wavelength and maximum output in power or energy and classified into four different classes. Accordingly, Class I lasers are very mild and safe. They include lasers used in everyday life; for example, those used in equipment that implement bar code scanning, such as cash registers at the supermarket. Class II lasers are in the visible light spectrum (400-700 nm). Some therapeutic lasers and laser pointers fall into this class. Damage can occur if the laser is directed into the eye for prolonged periods .
Class III lasers include the commonly used therapeutic lasers. These lasers are further subdivided into Class IIIB lasers are either continuous in the visible to the infrared spectrum or pulsed in the visible light spectrum. Class IIIR lasers are continuous within the visible light spectrum and have less power than Class IIIB lasers. Class IV lasers are the strongest lasers, and mostly include surgical lasers. They can permanently damage the eyes or burn the skin .
Types of laser
There are many types of lasers available for research, medical, industrial, and commercial uses (Table 1).
| Parameter | Types of lasers |
| Based on the medium they used | Gas Lasers |
| Crystal Lasers | |
| Semiconductors Lasers | |
| Liquid Lasers | |
| Based on the nature of emission | Continuous Wave |
| Single Pulsed Laser | |
| Repetitively Pulsed or scanning lasers | |
| Based on their wavelength | Visible Region |
| Infrared Region | |
| Ultraviolet Region | |
| Microwave Region | |
| X-Ray Region | |
| Based on different levels | 2-level laser |
| 3-level laser | |
| 4-level laser | |
| Based on the mode of pumping | Optical |
| Chemical | |
| Electric discharge | |
| Electrical | |
| Based on the sources | Dye Laser |
| Diode Laser | |
| Holmium Laser | |
| Excimer Laser | |
| Ruby Laser | |
| Argon Laser | |
| Argon Laser |
Table 1: List of different types of laser.
Source: https://ehs.oregonstate.edu/laser/training/laser-types-and-classification accessed on May 9, 2020.
Mechanism of laser therapy
The mechanism of action associated with photobiomodulation is often still questioned among scientists in the field. There are most likely several mechanisms of action depending on the target and the type of cell being modulated. Low-level laser therapy (LLLT), also known as photobiomodulation, is a painless treatment that uses clinically tested wavelengths of light to stimulate natural biological processes leading to faster healing and pain relief. Like plants absorbing sunlight through photosynthesis, cells in the body absorb laser energy that stimulates the body to release pain-relieving compounds, increases circulation, and energizes the cells to participate in the healing process. There are no side effects and many times laser therapy can take the place of pharmaceuticals and surgery to treat long-term, degenerative diseases .
The most published and recognized mechanism is that of the cytochrome c system, which is found in the inner cell membrane in the mitochondria and acts as a photoreceptor. Cytochrome C absorbs light from 500 to 1100 nm due to the specific properties of this large molecule. After laser light is absorbed by cytochrome C, it is excited and breaks bonds with nitric oxide (NO). This action allows bonding with oxygen to become more prevalent and cytochrome c oxidase to be produced at an optimal rate. Cytochrome c oxidase is critical to the formation of ATP. ATP is essential for energy production in the cell and results in many favorable biologic responses or secondary mechanisms, including reduction of pain and inflammation, and tissue healing .
A few studies have noted light to interact with the mitochondria in cells through cytochrome c oxidase and to generate reactive oxygen species, notably the superoxide anion O2 and its stable product (after the addition of two protons) hydrogen peroxide, H2O2 . In separate investigations, Burdon and Davies showed that a fairly small quantity of H2O2, approximately 0.1μmol to 0.5 μmol/107 cells, yielded bio-stimulatory effects. Recent reports on the biphasic characteristic of near-infrared 1,552 nm pulsed pico-second low time-average intensity radiation in suppressing the metabolic activity of the malignant human glioblastoma. The cellular metabolic activities for several fluence exposures were measured through the MTS metabolic assay. The addition of the enzyme catalase in the growth medium before the laser exposure was found to partially block the laser-induced metabolic suppression for the fluence values where maximum suppression was measured .
In the absence of catalase treatment conditions, the cellular metabolic activities to go from the control/sham-exposed levels to inhibition and back towards control levels. Whereas, in the presence of catalase (the effect of catalase is to scavenge hydrogen peroxide that permeated outside the cells) the reduction observed in the cellular metabolic activity is significantly mitigated, thus suggesting a functional role of H2O2 (Figure 1).

Figure 1: Mechanism of laser therapy in tissue.
Application of laser therapy in veterinary practice
Lasers therapy has been applied in different specialties procedures, practices, and devices. There appear to be many distinct benefits to using a therapeutic laser. These include angioplasty, cancer diagnosis, cancer treatment, dentistry, cosmetic dermatology such as scar revision, skin resurfacing, laser hair removal, tattoo removal, dermatology, to treat melanoma, frenectomy, lithotripsy, laser mammography, medical imaging, microscopy, ophthalmology (includes Lasik and laser photocoagulation), optical coherence tomography, optogenetics, prostatectomy plastic surgery, in laser liposuction, and in treatment of skin lesions (congenital and acquired) and in scar management (burns and surgical scars), surgery, and to cut, ablate, and cauterize tissue .
Moreover, laser light therapy can also be used in Neovascularization, Angiogenesis, Collagen synthesis which enhances wound healing, Stimulation of nerve healing, Enhanced healing of tendons, cartilage, and bones, reduce swelling from an injury, Modulation of degenerative tissue changes, and Mitigation of CNS damage following traumatic brain injury and spinal cord injury . The optimal wavelengths, intensities, and dosages for laser therapy in pets have not yet been adequately studied or determined, but this is sure to change as studies are designed and as more case-based information is reported. To maximize laser penetration, the pet’s hair should be clipped. When treating traumatic, open wounds, the laser probe should not contact the tissue, and the dose often quoted is 2 J/cm2 to 8 J/cm2 .
During the application of laser beams, it is recommended to hold the laser perpendicular (90 degrees) to the skin surface to minimize the reflection of the laser. Moreover, to minimize the scattering effect of the laser beams, the lasers should be applied directly to the skin that helps the beams to pass deeper into the tissue. For this purpose, using lasers having wavelengths in the range of 600 to 1200 nm. Besides, using lasers with larger spot areas allows more homogeneous passage of photons, and greater treatment area with less scatter of the beams .
When creating a treatment protocol for therapeutic laser, it is important to consider these effects to maximize patient outcomes. The actual time the tissue is exposed to light energy may also affect the outcome. Thus, proper application of laser therapy is not technically difficult, but it does require attention to be paid to basic technical principles, which can have profound effects on the success of treatment of the targeted tissue or area. Often, a lack of attention to these details is responsible for suboptimal outcomes .
Reducing inflammation
Laser energy increases the speed of tissue repair by increasing local microcirculation as well as stimulating the immune system and reducing inflammation . This is accomplished through a different mechanism. Among the possible mechanism of reducing pain are ATP production, stimulation of vasodilatation by induction of NO, reduction of interleukin-1, stabilization of cellular membranes, acceleration of leukocyte activity, decrease in prostaglandin, synthesis, lymphocyte response, angiogenesis, and superoxide dismutase (SOD) levels. All these actions may produce key elements that aid in the reduction of edema and inflammation .
Promoting heaing
The laser energy also enhances collagen and muscle tissue development, which in turn enhances healing . The traditional laser therapeutic studies showed that lasers have a wound-healing effect and the mechanisms of tissue healing are important for other injuries, such as tears and contusions of muscles, tendons, and ligaments, as many of the same mechanisms are needed to promote healing in all tissues. Besides, during laser treatment, physiological changes such as enhancing leukocyte infiltration , increased macrophage activity, increased neovascularization, increased fibroblast proliferation, keratinocyte proliferation, early epithelialization, increased growth factors, and increasing the wound tensile strength are seen .
Pain management
The therapeutic laser has been demonstrated to relieve both chronic and acute pain by modulating peripheral nerve function and nerve conduction velocities . The exact mechanisms remain unknown, but it is thought that laser therapy has the potential to influence pain perception by direct and indirect actions on superficial nociceptors and modulation of inflammation. Furthermore, repeated application of laser therapy may decrease central sensitization. Laser effects appear to be mainly inhibitory for pain receptors, and sensory nerves are more commonly affected. The superficial location of A-delta and C nerve fibers, along with neurons that supply the vasculature for vasoconstriction and vasodilation, allows laser penetration .
Several studies illustrate that photobiomodulation results in pain relief through various mechanisms. When laser interaction with cells, there will be increase in serotonin (5-HT) levels, increase in beta-endorphins, whose reception reduces the sensation of pain, increase in NO, which has an effect on vasodilatation and may enhance oxygen delivery, decreases bradykinins; bradykinins normally induce pain sensation by stimulating nociceptive afferent nerves, normalization of ion channels block depolarization of C-fiber afferent nerves, increase nerve cell action potential, and improve axonal sprouting and nerve cell regeneration .
LITHOTRIPSY IN DOGS AND CATS
“Lith” means stone and “tripsis” means crushing, thus, lithotripsy refers to breaking stones into small fragments to pass without incision of any part of the body. It is an alternative to surgical removal of urinary stone and it is less invasive. There are two types of lithotripsy: intracorporeal laser lithotripsy and extracorporeal shock wave lithotripsy. The gadget that breaks the stone or stones up is called a lithotriptor (also spelled lithotripter). With this technique, stones can be removed from the lower urinary tract (bladder and urethra). A specific type of laser called holmium: YAG laser, is used to break up the stone, and endoscopy is needed to get the laser right up to the stone where the patient’s tissues are not in the way .
If the stones are in the urethra, disruption of the stone is easiest. If the stones are in the urinary bladder, matters become more complicated. Issues that prevent success include the diameter of the urethra, hemorrhage obscuring the view of the stone or hampering the laser’s contact with the stone, accidental damage to the bladder from the laser, and prolonged anesthesia time because it is taking so long to fragment the stone(s). Despite these potential problems, studies have reported 83-96% success (i.e. complete stone removal) in female dogs and 68-81% success in male dogs .
If numerous stones are present, lithotripsy is not efficient and surgery should be performed instead. Some facilities recommend against lithotripsy if the pet has more than five stones. If the stones are large it may not be time-efficient to use lithotripsy (some facilities recommend against lithotripsy if there is more than one stone of a half-inch or more in diameter) .
Osteoarthritis
The anti-inflammatory effects of laser therapy are considered to be due to reduced levels of PGE2 and COX-2.10 In rat osteoarthritis (OA) models, laser therapy (1) reduced edema within the joint by 23%, (2) decreased vascular permeability in the periarticular tissue by 24%, and (3) decreased pain by 59%. Some subjective studies in humans with OA have shown (1) improved quality of life, (2) reduced pain, and (3) increased analgesic and microcirculatory effects .
Therefore, it has been suggested that individual results may depend on the type and extent of disease, wavelength, method of application, dosage, site, duration of treatment, and tendon and ligament conditions. Treatment of osteoarthritis (OA) in dogs and cats using a therapeutic laser is commonly described. The laser dose that may be most appropriate in OA is 8 J/cm2 to 10 J/cm2 applied as part of a multi-modal arthritis treatment plan. Finally, tendonitis may benefit from laser therapy due to the inflammation associated with the condition .
An experimental study in rats with calcaneal lesions treated with laser therapy revealed improved collagen organization in the treatment group compared with the control group, with 5-day treatment providing an optimal response. In humans, results are conflicted, with about 50% of studies showing a positive effect and 50% showing no effect. In human ligamentous injuries, laser therapy has shown improved tensile strength and stiffness compared with controls .
Tumor or cancer treatment
The study performed on 38 privately-owned dogs to remove different types of skin tumors using CO2 laser techniques revealed different outputs. The treatment effect was based on the surgical wound evaluation, the relative time of healing, and possible local recurrence of the tumor after 3 months post-surgery. Local recurrence was observed in two cases. The study showed that in 30 cases time needed for complete resection of lesions was less than 10 minutes. The time of healing was longer than 12 days in 6 cases (42.8%) with tumor excision and in 14 cases (87.5%) where excision with ablation technique was performed. In conclusion, the advantages of the CO2 laser surgery were better hemostasis, the precision of working, non-contact dissection, fewer instruments at the site of operation, and minimum traumatization of the surrounding tissues .
APPLICATION IN LASER SURGERY
Surgical and therapeutic use of lasers began in human medicine in the early 1960s. Over the last ten years, with rapid advancements in technology and equipment, veterinarians have been exploring the many potential advantages of lasers and veterinary patients were benefited from these lasers. Because laser light energy can be applied directly to the target tissue or administered to distant lesions at a remote site through fiberoptic components, laser surgery has become an invaluable and growing veterinary surgical resource. Unlike many medical technologies, the size, reliability, and portability of lasers have improved so rapidly that they are now both economically and practically feasible for the general and specialty veterinarian .
Routine laser use in veterinary medicine stands poised to gain large-scale general acceptance for everyday routine and specialty procedures. When treating a post-operative incision, a dose of 1 J/cm2 to 3 J/ cm2 per day for the first week after surgery is described. Lick granulomas may benefit from therapeutic laser once the source of the granuloma is identified and treated .
Currently, the most efficient way to determine the dose and time is to use available treatment (Table 2).
| Disease condition | Treatment | Therapeutic dose |
| Joint Pain | Analgesia or anti-pain | |
| Acute pain | 4-6 J/ cm2 per day | |
| Chronic pain | 4-8 J/ cm2 per day | |
| Muscle pain | Analgesia or anti-pain | |
| Acute pain | 2-4 J/ cm2 per day | |
| Chronic pain | 4-8 J/ cm2 per day | |
| Inflammation | Anti-inflammatory therapy | |
| Acute Inflammation | 1-6 J/ cm2 per day | |
| Chronic Inflammation | 4-8 J/ cm2 per day | |
| Open wound | Open wound management | |
| Acute wound | 2-6 J/ cm2 for 7-10 days | |
| Chronic wound | 2-8 J/ cm2 per day | |
| Osteoarthritis | Joint line therapy | 8-10 J/ cm2 depends on the type of joint |
| Post-surgical wound | Wound management | 1-3 J/ cm2 per day |
Table 2: Treatment guidelines for different disease condition using laser therapy. Source: .
Laser safety procedures
There are some important safety considerations when incorporating therapeutic laser into treatment protocols. Generally, precautions with laser therapy involve protecting the eyes with protective glasses with lenses rated to the specific wavelength of the treatment lasers are important for both humans and animals to protect retinal tissue. Since the light is coherent, a small amount focused on the retina may cause permanent damage. Fortunately, visible light will generate a blink reflex to help protect the user; however, infrared lights are not visible so a blink reflex will not occur. All necessary care should be taken if the pet has a tattoo, black fur, or black skin because of the potential for light absorption and tissue heating .
Contraindications to direct laser treatment include carcinoma, thyroid gland, active hemorrhage, and autonomic nerve centers. Laser energy should not be applied over a pregnant uterus, over tumors, over an open fontanel, over the growth plates of immature animals, malignancies, and photosensitive areas of the skin. Laser therapy should be avoided in patients in which immune stimulation is not desired, including those with lymphoma or on immunosuppressant medications. In immature patients, higher-powered laser therapy devices may stimulate premature closure of epiphyses. Thus, caution is warranted over long bones in animals less than 1-year old .
Future perspective of laser therapy
Therapeutic laser is of special interest in the area of nerve regeneration, particularly in human medicine. Veterinary patients experience peripheral nerve issues as they age, as osteoarthritis develops and progresses, in the wake of intervertebral disk disease, and when they develop nervous system decline as occurs in degenerative neuropathy/myelopathy. Photobiomodulation has been demonstrated to support nerve regeneration, re-innervation of denervated muscle, and functional recovery following peripheral nerve injury. This is an area of active research that promises to provide a significant impact on both human and veterinary patients.
Lasers have significant measurable effects on living tissues in laboratory experiments. Preclinical research, while inconsistent, also suggests potential benefits. Extensive research done in humans has so far produced limited evidence to support the use of lasers in a few conditions. Experimental evidence in veterinary species is mixed, and there are no systematic reviews of clinical trials validating laser therapy for specific indications. Hopefully, future research will clarify the benefits of laser therapy, identifying which techniques are useful for which conditions and in what circumstances laser treatment is not beneficial.
WHEN SHOULD LASER THERAPY BE USED?
While veterinary studies are sparse, currently, most studies evaluating laser therapy focus on wound healing and pain management.
From a biologic perspective, photons absorbed through cellular pathways allow production of adenosine triphosphate (ATP). This process is similar to photosynthesis in plants: light is absorbed and converted into chemical energy (ATP) by reduction of CO2 to useful organic compounds, such as glucose.
ATP not only alters cellular metabolism, but also acts as a cell-signaling molecule and/or neurotransmitter.
- ATP’s role as a neurotransmitter helps explain some of the pain modulationeffects of lasers.
- Due to enhanced cellular metabolism, lasers potentially accelerate tissue repairand cell growth.
- Additional effects of laser therapy are stimulation of stem cells and anti-inflammatory effects that decrease prostaglandin E2 (PGE2) and cyclooxygenase-2 (COX-2).
Further, in-depth discussion of biochemical reactions is beyond this article’s scope.
Osteoarthritis
The anti-inflammatory effects of laser therapy are considered to be due to reduced levels of PGE2 and COX-2.10 In rat osteoarthritis (OA) models, laser therapy (1) reduced edema within the joint by 23%, (2) decreased vascular permeability in the periarticular tissue by 24%, and (3) decreased pain by 59%.
Some subjective studies in humans with OA have shown (1) improved quality of life,2 (2) reduced pain, and (3) increased analgesic and microcirculatory effects.12 However, there have been conflicting reports in human medicine that reveal no benefits of laser therapy.1
Therefore, it has been suggested that individual results may depend on:
- Type and extent of disease
- Wavelength
- Method of application
- Dosage
- Site
- Duration of treatment.
Tendon & Ligament Conditions
An experimental study in rats with calcaneal lesions treated with laser therapy revealed improved collagen organization in the treatment group compared with the control group, with 5-day treatment providing optimal response.
In humans, results are conflicted, with about 50% of studies showing a positive effect and 50% showing no effect. In human ligamentous injuries, laser therapy has shown improved tensile strength and stiffness compared with controls.
Pain Management
The exact mechanisms remain un-known, but it is thought that laser therapy has the potential to influence pain perception by direct and indirect actions on superficial nociceptors and modulation of inflammation. Furthermore, repeated application of laser therapy may decrease central sensitization.
Laser effects appear to be mainly inhibitory for pain receptors, and sensory nerves are more commonly affected.1 The superficial location of A delta and C nerve fibers, along with neurons that supply the vasculature for vasoconstriction and vasodilation, allows laser penetration.
Unfortunately, use of lasers for pain management is purely speculative due to lack of studies. Hopefully, more evidence will become available in the future.
KEY RECOMMENDATIONS
- Hold the laser 90 degrees to the skin surface to minimize reflectionof the laser.
- To help negate the scatter effect, use wavelengths in the range of 600 to 1200 nm, which pass deeper into tissue and minimize this effect, and apply the laser directly to the skin.
- Use lasers with larger spot areas, which allow more homogeneous passage of photons, less scatter, and greater treatment area.
HOW IS LASER THERAPY APPLIED?
To treat small areas, laser therapy is administered using a handheld probe with a beam. The probe can be placed in:
- Direct contact with the skin, which minimizes reflection of photons (Figure 5)
- A noncontact position, in which the probe is held perpendicular to the treatment area and off the skin (Figure 6). Noncontact is recommended for wound treatment.
Dose & Duration
Currently, the most efficient way to determine the dose and time is to use available treatment tables1 (Table).

Step-by-Step Application
- Clip the patient’s hair, which maximizes the laser’s effect because hair absorbs 50% to 90% of the light.
- Measure the area to be treated.
- Determine the treatment dose; in areas of darker skin, the dose should be increased by 25%.
- Determine the total joules (J/cm2) and treatment time needed. For example: If treating an area of 57 cm2(size of a playing card) with 10 J/cm2, the total treatment is 600 J. If using a 10-W laser, the treatment time is 60 seconds.
- Place safety goggles prior to using the laser: all personnel in the room should wear protective eye gear, and the patient’s eyes should also be protected.
- The laser should be pointed perpendicular to the treatment area.
- Apply the laser treatment, moving slowly, over the area by using an overlapping grid technique to ensure the entire area is treated.
Precautions
Precautions with laser therapy generally involve protecting the eyes during treatment. Since the light is coherent, a small amount focused on the retina may cause permanent damage. Fortunately, visible light will generate a blink reflex to help protect the user; however, infrared lights are not visible so a blink reflex will not occur.
Contraindications & Precautions to Laser Therapy
- Always use protective eye gear; furthermore, eyewear should be appropriate for the wavelength of the laser being used.
- Never direct the laser into the eye.
- Use caution around metal surfaces as they can cause scatter of the laser light.
- Use caution with the following: pregnancy, open fontanels, around growth plates, malignancies, and photosensitive areas of the skin.
- Darker skin and hair can absorb the laser light and cause excessive heating of the skin.
In general, laser therapy is an emerging technique that appears to at least have subjective benefits and it is an increasingly studied modality that can be a valuable tool for veterinary practitioners to successfully treat conditions. Potential areas where laser therapy can be incorporated are in wound healing, pain management, and rehabilitation for various conditions (eg, Osteoarthritis). Mechanisms of action have been studied and identified for the reduction of pain and inflammation, as well as the healing of tissue. Understanding the basics of light penetration into tissue allows evaluation of the correct dosage to deliver for the appropriate condition, as well as for a particular patient based on physical properties. Photobiomodulation has several potential benefits and regularly using this technology may allow for the discovery of other applications. New applications are currently being studied for some of the most challenging health conditions and this field will continue to grow as we learn more. Additional clinical studies are needed and collaboration is highly encouraged for all practitioners using this technology. There are a growing number of educational resources about therapeutic lasers and recent advances.
Photo courtesy-RUBY LYNN CARTER
1 School Of Veterinary Medicine, Wolaita Sodo University, P. O. Box 138, Wolaita Sodo, Ethiopia
*Corresponding Author(s):
Haben Fessehav
School Of Veterinary Medicine, Wolaita Sodo University, P. O. Box 138, Wolaita Sodo, EthiopiaSource-https://www.heraldopenaccess.us/openaccess/laser-therapy-and-its-potential-application-in-veterinary-practice-a-review
REFERENCES
- Smith KC (2010) Laser and LED photobiology. Laser Therapy 19: 72-78.
- Bartels KE (2002) Lasers in medicine and surgery. Veterinary Clinics: Small Animal Practice 32: xiii-xv.
- Millis DL, Saunders DG (2014) Laser therapy in canine rehabilitation. In Canine rehabilitation and physical therapy pg no: 359-380.
- Peplow PV, Chung TY, Baxter GD (2010) Laser photobiomodulation of wound healing: A review of experimental studies in mouse and rat animal models. Photomedicine and laser surgery 28: 291-325.
- Pryor B, Millis DL (2015) Therapeutic laser in veterinary medicine. Veterinary Clinics: Small Animal Practice 45: 45-56.
- Naeser MA, Hamblin MR (2011) Potential for transcranial laser or LED therapy to treat stroke, traumatic brain injury, and neurodegenerative disease. Photomedicine and Laser Surgery 29: 443-446.
- Roberts DB, Kruse RJ, Stoll SF (2013) The effectiveness of therapeutic class IV (10 W) laser treatment for epicondylitis. Lasers in surgery and medicine 45: 311-317.
- Yasukawa A, Hrui H, Koyama Y, Nagai M, Takakuda K (2007) The effect of low reactive-level laser therapy (LLLT) with helium-neon laser on operative wound healing in a rat model. J Vet Med Sci 69: 799-806.
- Calin MA, Coman T (2011) The laser in veterinary medicine. Turkish Journal of Veterinary and Animal Sciences 35: 351-357.
- da Silva JP, da Silva MA, Almeida APF, Júnior IL (2010) Laser therapy in the tissue repair process: A literature review. Photomedicine and laser surgery 28: 17-21.
- Berger NA, Eeg PH (2006) Veterinary laser surgery: A practical guide. Wiley Online Library, USA. Pg no: 234.
- Draper WE, Schubert TA, Clemmons RM, Miles SA (2012) Low?level laser therapy reduces time to ambulation in dogs after hemilaminectomy: A preliminary study. Journal of Small Animal Practice 53: 465-469.
- Paczuska J, Kie?bowicz Z, Nowak M, Anto?czyk A, Ciaputa R, et al. (2014) The carbon dioxide laser: An alternative surgery technique for the treatment of common cutaneous tumors in dogs. Acta Acta Vet Scand 56: 1.
- Winkler CJ (2019) Laser Surgery in Veterinary Medicine. Wiley Online Library, USA.
- Ali MR, Ibrahim IM, Ali HR, Selim SA, El-Sayed MA (2016) Treatment of natural mammary gland tumors in canines and felines using gold nanorods-assisted plasmonic photothermal therapy to induce tumor apoptosis. Int J Nanomedicine 11: 4849-4863.
- Galli A, Giordano L, Sarandria D, Di Santo D, Bussi M (2016) Oncological and complication assessment of CO2 laser-assisted endoscopic surgery for T1-T2 glottic tumours: Clinical experience. Acta Otorhinolaryngologica Italica 36: 167.
- Tata DB, Waynant RW (2011) Laser therapy: A review of its mechanism of action and potential medical applications. Laser & Photonics Reviews 5: 1-12.
- Farivar S, Malekshahabi T, Shiari R (2014) Biological effects of low level laser therapy. J Lasers Med Sci 5: 58.
- Anders JJ, Moges H, Wu X, Erbele ID, Alberico SL, et al. (2014) In vitro and in vivo optimization of infrared laser treatment for injured peripheral nerves. Lasers Surg Med 46: 34-45.
- Bjordal JM (2012) Low level laser therapy (LLLT) and World Association for Laser Therapy (WALT) dosage recommendations. Photomed Laser Surg 30: 61-62.
- Smith JJ (2017) General principles of laser therapy. In: Riegel RJ, et al. (eds.), Laser therapy in veterinary medicine. Pg no: 55-66.
- Kronberger C (2002) The veterinary technician’s role in laser surgery. Vet Clin North Am Small Anim Pract 32: 723-735.
- Tomasello AJ, Graveman W, Dowlatshahi K, Appelbaum HR (2019) Interstitial laser therapy control system. Google Patents.
- Gilmour MA (2002) Lasers in ophthalmology. The Veterinary clinics of North America. Small Animal Practice 32: 649-672.
- Millis DL, Francis D, Adamson C (2005) Emerging modalities in veterinary rehabilitation. Vet Clin North Am Small Anim Pract 35: 1335-1355.
- Arany P (2011) Laser photobiomodulation: models and mechanisms. Journal Laser Dentistry: 19.
- Tuner J, Hode L (2010) Some basic laser physics, Therapeutic lasers. The New Laser Therapy Handbook. Sweden: Prima books AB. Pg no: 1-47.
- Hamblin MR, Demidova TN (2006) Mechanisms of low level light therapy. In Mechanisms for low-light therapy 614001: 1-12.
- Tuner J, Hode L (2010) The new laser therapy Handbook: A guide for research scientists, doctors, dentists, veterinarians and other interested parties within the medical field. Prima Books AB.
- Kameya T, Ide S, Acorda JA, Yamada H, Taguchi K, et al. (1995) Effect of different wavelengths of low level laser therapy on wound healing in mice. Laser Therapy 7: 33-37.
- Ferreira I, Ferreira J, Vollet-Filho JD, Moriyama LT, Bagnato VS, et al. (2013) Photodynamic therapy for the treatment of induced mammary tumor in rats. Lasers in medical science 28: 571-577.
- Gerdes HM (2002) Method and apparatus for therapeutic laser treatment. Google Patents.
- Karoussis IK, Kyriakidou K, Psarros C, Koutsilieris M, Vrotsos JA (2018) Effects and Action Mechanism of Low Level Laser Therapy (LLLT): Applications in Periodontology. Dentistry 8: 514.
- Sacu S, Schmidt-Erfurth U (2014) Principles of laser therapy. Clinical Ophthalmic Oncology. Pg no: 83-88.
- Wardlaw JL, Gazzola KM, Wagoner A, Brinkman E, Burt J, et al. (2019) Laser therapy for incision healing in 9 dogs. Front Vet Sci 5: 349.
- Seaton ED, Mouser PE, Charakida A, Alam S, Seldon PM, et al. (2006) Investigation of the mechanism of action of nonablative pulsed?dye laser therapy in photorejuvenation and inflammatory acne vulgaris. Br J Dermatol 155: 748-755.
- Yang Z, Wu Y, Zhang H, Jin P, Wang W, et al. (2011) Low-level laser irradiation alters cardiac cytokine expression following acute myocardial infarction: A potential mechanism for laser therapy. Photomed Laser Surg 29: 391-398.
- Lucroy MD, Edwards BF, Madewell BR (1999) Low?intensity laser light?induced closure of a chronic wound in a dog. Veterinary Surgery 28: 292-295.
- Davidson EB, Ritchey JW, Higbee RD, Lucroy MD, Bartels KE (2004) Laser lithotripsy for treatment of canine uroliths. Vet Surg 33: 56-61.
- Goldman JA, Chiapella J, Casey H, Bass N, Graham J, et al. (1980) Laser therapy of rheumatoid arthritis. Lasers Surg Med 1: 93-101.
- Woodruff LD, Bounkeo JM, Brannon WM, Dawes KS, Barham CD, et al. (2004) The efficacy of laser therapy in wound repair: A meta-analysis of the literature. Photomedicine and laser surgery 22: 241-247.
- Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, et al. (2005) Low?level laser therapy for wound healing: mechanism and efficacy. Dermatologic surgery 31: 334-340.
- Anders JJ, Geuna S, Rochkind S (2004) Phototherapy promotes regeneration and functional recovery of injured peripheral nerve. Neurological research 26: 233-239.
- Ottaviani G, Martinelli V, Rupel K, Caronni N, Naseem A, et al. (2016) Laser therapy inhibits tumor growth in mice by promoting immune surveillance and vessel normalization. EBioMedicine 11: 165-172.
- Jako GJ (1985) Laser surgery. Google Patents.
- Dycus D (2014) Laser Therapy in Companion Animals What It Is, How It Works, & When It Benefits Patients. Today’s Veterinary Practice. Pg no: 61-65.
- Bajaj PKL, Chopra R (2015) Laser dentistry & safty prospectus-a review. International Journal of Oral Health Sciences and Advances 3: 27-33.
- Bartels KE (2017) Therapy Laser Safety. In: Riegel RJ, et al. (eds.), Laser Therapy in Veterinary Medicine: Photobiomodulation, Wiley Online Library, USA.