CYSTICERCOSIS (PORK TAPEWORM INFECTION): AN EMERGING PARASITIC HUMAN DISEASE IN INDIA
Cysticercosis, popularly known as Tapeworm [Taenia solium] infection, is a very common disease where the patient would have consumed food or water infested with tapeworm eggs or larvae. These grow into adult tapeworms that cause an invasive infection by forming cysts in body tissues and organs outside the intestines or an intestinal infection by growing right inside the intestines. Cysticercosis caused by larval stage of the tapeworm Taenia solium, is a major public health problem, especially in the developing world. Neurocysticercosis (NCC) is considered to be the most common parasitic infestation of the central nervous system (CNS) and the single most common cause of epilepsy in the developing countries (Garcia et al 2003; Prasad et al 2008b). Three quarters of the estimated 50 million people with epilepsy live in the poor countries of the world and up to 94% of them remain untreated (Bertellote et al 1994). Human is the only defi nitive host of T. solium harbouring adult tapeworm in the intestine (taeniasis), where as both man and pig can act as intermediate hosts and harbour the larvae in different internal organs (cysticercosis) including brain (NCC). Human and pig both acquire cysticercosis through ingestion of eggs excreted in faeces by human T. solium carrier. T. solium infection is also increasingly diagnosed in affl uent countries owing to human migration from endemic areas (Garcia et al 1996). Cysticercosis is common in communities where pigs are allowed to roam freely, the residents consume undercooked pork and the basic sanitary facilities are lacking (WHO 1983; Prasad et al 2007).
These adult tapeworms have a head, neck and a series of segments called proglottids. A person with intestinal infection will have the tapeworm head stuck to the intestinal wall where the proglottids grow and multiply more eggs. At a given time, such tapeworms can live up to 30 years in the host.The clinical conditions caused by Taenia solium are classified as either Cysticercosis (cysts in various tissues including the brain) or Taeniasis (intestinal tapeworm infection).
Taeniasis is usually mild, though persistent tapeworm infection can result in serious complications.Cysticercosis is originates from the metacestode, (larval stage of Taenia solium), the pork tapeworm.Neurocysticercosis refers to CNS infection with T solium. Neurocysticercosis is further classified into parenchymal and extraparenchymal disease. Parenchymal disease is distinguished by existence of cysticerci within the brain parenchyma. Extraparenchymal disease develops when cysticerci progress to the CSF of the ventricles, cisterns, and subarachnoid space or are seen within the eyes or spinal cord.
Disease burden in India
All the biological markers for transmission of T. solium taeniasis and cysticercosis exist in India. It is likely that the disease is under reported in India because due attention has not been given to this neglected disease and systematic population-based studies are lacking. There are great disparities within the country in geography, ethnicity, religion rituals, income, food habits, personal hygiene, level of education and standards of living, which are likely to infl uence the disease burden. Consequently there are wide variations in the frequency of cysticercosis in India (fi gure 1). There are only few reports from the State of Kerala, where the level of education and standards of hygiene are high, and from Jammu and Kashmir, a Muslim majority State due to prohibition of pork consumption by religion. Before the era of CT scan and magnetic resonance imaging (MRI), National Institute of Mental Health and Neuro Sciences (NIMHANS), Bangalore reported diagnosis of NCC in 2% of an unselected series of epileptics (Mani et al 1974). At a tertiary referral centre in New Delhi, NCC constituted 2.5% of all intracranial space occupying lesions (Wani et al 1981). With the availability of CT and MRI, the proportion of NCC in seizure disorders dramatically increased. Sawhney et al (1996) reported cerebral cysticercosis in 31% of patients in whom CT was done. In a community survey of 50,617 individuals from South India, the prevalence of active epilepsy was 3.83 per 1000 and NCC was detected in 28.4% of them by CT (Rajshekhar et al 2006). Cysticercosis appears to be more prevalent in the northern States Bihar, Uttar Pradesh through Punjab. In a recent study based on 30 cluster sampling approach suggested by WHO in the rural pig farming community of Mohanlalganj block, Lucknow district, Uttar Pradesh, the prevalence of taeniasis was 18.6%; factors associated with taeniasis were age above 15 years, history of passage of Taenia segment in stool, undercooked pork consumption and poor hand hygiene (Prasad et al 2007). In the same community active epilepsy was identifi ed and clinically confi rmed in 5.8% of the populations during door to door survey and 48.3% of them fulfi lled either defi nitive or probable diagnostic criteria of NCC. Epilepsy in the family and no separate place for pig were identifi ed as risk factors for NCC clustering (Prasad et al 2008b). The single cyst infection (range 47.7% to 53.4%), is the most common in Indian subcontinent (Prasad et al 2008a; Prabhakaran et al 2007). In a study of 156 histologically proven cases of cysticercosis from Patiala, Punjab, 88% patients presented with solitary lesion and the most frequent site being the upper arm, chest wall, eye, abdomen wall and neck (Saigal et al 1984). In a seroprevalence study in and around Chandigarh, anti-cysticercus antibodies was found to be 17.3% with highest prevalence (24%) reported from slum areas; however only 8% of the sero-postives had previous history of seizure (Khurana et al 2006; Saigal et al 1984). Cysticercosis sero-prevalence among the healthy blood donors from Pondicherry was 6.5% using both antigen and antibody detection methods (Parija et al 2005). The prevalence of taeniasis ranged from 0.5-2% in hospitalized patients in northern India, 12–15% in labour colonies where pigs are raised (Mahajan et al 1982). The treatment gap in rural India is above 90% (Prasad et al 2008b) and the probable reasons for such high gap are socioeconomic, lack of knowledge and medical facilities, social prejudice to modern medicine and faith in alternative treatment modalities. Cysticercosis also appears to be widespread among swine in India. In and around Chandigarh, 8–10% of the pigs slaughtered had cysticerci in their muscles and around 0.5% of the pigs reared in Government farms were found to be infected (Mahajan et al 1982). Another survey in slaughter houses of Kolkata (West Bengal) revealed cysticercosis in muscles of 7% of the slaughtered pigs (Ratnam et al 1983). Prasad et al (2002) reported a high frequency of cysticercosis (26%) in swine from Mohanlalganj block of Lucknow district in the State of Uttar Pradesh and 40% of them had cysticerci in the brain.
Cysticercosis Symptoms
Usually, people with cysticercosis do not display any symptoms. It is actually the effects of the infection that lead people to go to doctors. Also, the type of infection and tapeworm, and the extent of infection and location determine most symptoms.
Intestinal Tapeworm Infection [Taeniasis]
Symptoms include
- Nausea
- No appetite
- Abdomen – twinges of discomfort
- Diarrhea
- Weakness
- Weight loss
- Poor absorption of nutrients from food
Invasive Tapeworm Infection [Cysticercosis]
Besides cysts formation and causing organ and tissue damage, invasive larval infection results in the following symptoms:
Symptoms of cysticercosis may include seizures, elevated intracranial pressure (ICP), meningoencephalitis, psychiatric disorder, stroke, and/or radiculopathy or myelopathy, if the spinal cord is concerned.
The symptoms are primarily due to the effect of a mass, an inflammatory reaction, or impediment of the foramina and ventricular system of the brain. The most familiar symptoms include seizures, focal neurologic signs, and intracranial hypertension.
Parenchymal CNS Disease
- Seizures may be focal, focal with secondary generalization, or generalized.
- Headaches are regular and may be like a migraine.
- Neurocognitive deficits, while exceptional, may include learning disabilities, depression, or even neurosis.
Extraparenchymal Disease
- Most patients appear to have headaches or symptoms of hydrocephalus.
- Symptoms of augmented ICP may include headache, nausea or vomiting, distorted mental state, giddiness, and diminished visual acuity due to papilledema.
- Patients with numerous cysticerci in the basilar cisterns may build up communicating hydrocephalus, meningismus (without fever), signs of lacunar infarcts due to small-vessel vasculitis, or symptoms of large-vessel infarcts due to cysticercal corrosion into major arteries or rigorous inflammation of those arteries.
Those with spinal cysticerci typically appear with radicular symptoms, but rarely with motor or sensory shortage observable to a spinal level.
Cysticercosis Risk Factors
The following conditions put one to great risk of Taeniasis and Cysticercosis:
- Poor hygiene and sanitationLack of the habit of bathing and not washing hands frequently and correctly with soap and water exposes one to consumption of contaminated matter that may contain larvae or eggs of tapeworm.
- Exposure to cattle and livestock Those having to deal with animal and human feces in farms and otherwise, are at great risk of contracting this infection.
- Consumption of raw and uncooked meatsPoorly cooked meats do not kill the larvae or eggs attached to them thus increasing the risk of infection.
- Residing/travel in endemic countriesCertain parts of Latin America, China, sub-Saharan Africa and South East Asia have a greater exposure tendency to tapeworm infection where pigs roam freely. If one happens to live/travel to these places, chances are high that one might contract this infection.
Life cycle, biology, and transmission————
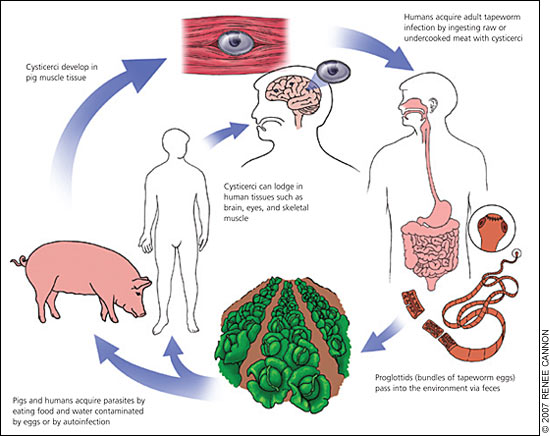
Life cycle of T. solium comprises two natural hosts, humans as the defi nite and swine as the intermediate host. Human harbours the adult tapeworm; eggs produced by the worm are disseminated to the environment through faeces. The pig ingests some of these eggs, which develop into cysticerci in internal organs like muscle and brain. When human consumes contaminated pork containing cysticerci, they develop into an adult worm in the small intestine (fi gure 2). The adult worm attaches itself to the intestinal mucosa by scolex equipped with four lateral suckers and a rostellum, which bears 25-50 hooklets. T. solium is a hermaphrodite and the gravid proglottides, containing the eggs reach the environment by passive discharge in the faeces. The eggs are spherical and measure 30-40 μm in diameter. After being liberated from the proglottides, the eggs can be ingested by swine and man. Once in the digestive tract, the eggs lose their coat by gastric and pancreatic enzymes and liberate hexacanth embryos or oncospheres. Aided by their hooklets, the oncospheres cross the intestinal wall and local venules, enter systemic circulation and are carried to different organs of the host (skeletal muscles, CNS, subcutaneous tissue, eye, etc.). Here the oncospheres lose their hooklets, acquire a vesicular shape and evolve into cysticerci by gradual evagination of the protoscolex (invaginated scolex) over a period of two months (Escobar and Neito 1972). The life cycle is completed when undercooked pork infested with cysticerci is eaten by human beings. However, man may also become an intermediate host and develop the larval stage of the disease in one of the ways: (i) by heteroinfection, the most common route, in which eggs present in food contaminated by the faeces of Taenia carriers are ingested; (ii) by exogenous autoinfection, due to ano-oral contamination in patients harbouring the adult worm; (iii) by endogenous autoinfection, in which the eggs of the adult tapeworm living in the small intestine return to the stomach due to reverse peristalsis. The last two modes of autoinfection are far less frequent as it is quite uncommon to fi nd patients having simultaneous infestation with cysticercosis and taeniasis in more than 10-15% cases (Rabiela-Cervantes et al 1982). In humans, parasite may get lodged in the CNS and results in NCC (Del Brutto and Satelo 1988). The larval stage also infests other tissues like skeletal muscle, diaphragm, heart and peritoneum, pleura and subcutaneous tissue (Shankar et al 1994). Mammals other than swine have also been reported to harbour cysticerci of T. solium. In Indonesia, examination of two sero-positive dogs revealed cysticerci of T. solium in their brain and heart (Ito et al 2002). C. cellulosae have also been recovered from the brain of a cat (Schwan et al 2002).
Cysticercosis Diagnosis
The diagnosis is fairly simple and the doctor will ask for the following tests:
- Stool analysis Doctors and labs may ask for more than one stool sample to check for the presence of tapeworm eggs and the extent of infection.
- Blood sample Once the infection has invaded tissues, doctors will ask for a blood sample to check antibodies in the blood which definitely indicate presence of infection.
- Imaging tests A CT scan or MRI, X-ray or an Ultrasound is required to confirm invasive tapeworm infection and the presence of cysts.
Cysticercosis Treatment
Treatment of NCC– Treatment for NCC with antihelminthic drugs (AHDs) such as metriphonate, mebendazole, fl ubendazole, praziquantel and albendazole were published more than 15 years ago, but clinical trials to establish the specifi c indications, defi nite doses, and duration of treatment are lacking. Some authors suggest that control of seizures in patients with NCC is better fter a course of anticysticercal drugs (Garcia et al 2004; Medina et al 1993) and that the chance of remaining seizure free after the withdrawal of anti-epileptic drugs (AEDs) seems to be greater in those patients who were previously treated with AHDs (Del Brutto et al 1996). Albendazole and praziquantel effectively destroy the cerebral parenchymal cystic lesions. Albendazole is possibly more effective in subarachnoidal, ventricular and spinal cysticercosis, and frequently obviates the need for surgery. Recently, there is an intense debate on usefulness and safety of anticysticercal treatment (Singh and Sander 2004). Opponents of anticysticercal therapy argue that effectiveness of therapy is possibly a refl ection of natural course of the disease and even if cysticercal lesions are left untreated, they either disappear spontaneously or are calcifi ed (Mitchell and Crawford 1988; Kramer et al 1989). Anticysticercal therapy may aggravate cerebral edema, produce vasculitis and stroke, which may even lead to death. To minimize these risks, concomitant corticosteroids is administered especially if there is a massive parasitic load. Anticysticercal treatment is avoided in patients with cysticercotic encephalitis (Del Brutto and Sotelo 1988; Carpio et al 1998). There was a strong consensus that there is no role for antiparasitic drugs in patients with only calcifi ed lesions (Riley et al 2003). Most experts strongly recommend antiparasitic therapy in patients with multiple subarachnoid cysticerci or giant cysticerci.
Once diagnosed with infection, doctors usually prescribe oral medicines to kill the tapeworm presence including larvae and follow it up with a stool examination which should not have tapeworm, larva or proglottids to double check that one is clear of the infection.The effect of oral medications prescribed depends a lot on the type of tapeworm infection detected and the site of infection. The idea is to not re-infect oneself and therefore, hand sanitation and hygiene becomes very important.
Treatment for invasive tapeworm infection also depends on the type of tapeworm detected and the extent and site of infection- anthelminthic drugs, anti-inflammatory therapy, anti-epileptic therapy, shunt placement and surgery.
Neurocysticercosis treatment should be based on each individual and whether cysts are nonviable or active, which usually can be assessed by neuroimaging studies such as MRI or CT, and where they are located.
For patients with only nonviable cysts, treatment should be indicative and contain anticonvulsants for individuals with seizures and shunting for patients with hydrocephalus.
Corticosteroids are specified for all patients with multiple cysts and associated cerebral edema (“cysticercal encephalitis”). Hydrocephalus shunting is also important.
Ocular cysticercosis also is attended to by surgical elimination of the cysts, but not generally with antihelmintihc drugs, which could exacerbate ocular inflammation.
Prevention and control
Cysticercosis has been recognized as a potentially eradicable disease. The main method of control in developed countries has been the eradication of swine cysticercosis through improved animal husbandry and meat inspection procedures. This approach has resulted in the successful interruption of transmission of intestinal T. solium in the United States and Western Europe (Ferreira et al 1997). A small number of individuals with tapeworm may infect vast numbers of healthy human beings. Tapeworm carriers are an appealing target for the control of cysticercosis/taeniasis. In the developing world, emphasis has been placed on control of the parasite through health education and mass administration of antihelminthic drugs in areas of endemicity in an attempt to remove tapeworm carriers (Plancarte et al 1999; Garcia et al 2003; Lightowlers 2003).
Till date no vaccine has been developed against the T. solium although many groups had reported the success of a few proteins in vaccination of porcine cysticercosis. However the complex immunology of the parasite, occult nature of this infection and the minimal morbidity associated with this infection, make taeniasis a poor candidate for vaccine development. Vaccination against taeniasis does not, therefore, appear to be immunologically or logistically feasible at the present. Vaccinating pigs in endemic region to prevent porcine cysticercosis may be good strategy to improve animal health, meat yield and to break the parasite life cycle, preventing taeniasis and consequently preventing human cysticercosis. In laboratory and fi eld studies, a variety of antigens have demonstrated effective partial protection (Lightowlers 2003). A protective antigen from Taenia ovis oncosphere-stage has been cloned to develop a recombinant vaccine for ovine cysticercosis and this vaccine is available commercially for veterinary use in New Zealand (Rickard et al 1995). On the basis of evidence of a similar immune response to T. solium, it should also be possible to develop an effective vaccine to prevent both human and swine cysticercosis (Mitchell and Crawford 1997). It has been proposed to develop a safe, effective, inexpensive vaccine for swine, which can be administered in an edible form (Eddi et al 2003).
FAQ ON TAENIASIS
What is taeniasis?
Taeniasis is an infection caused by the tapeworm, a type of parasite. Parasites are small organisms that attach themselves to other living things in order to survive. The living things the parasites attach to are called hosts.
Parasites can be found in contaminated food and water. If you consume contaminated food or drinks, you may contract a parasite that can live and sometimes grow and reproduce inside your body.
Taeniasis is an intestinal tapeworm infection caused by eating contaminated beef or pork. It’s also known by the following names:
- Taenia saginata (beef tapeworm)
- Taenia solium (pork tapeworm)
What are the symptoms of taeniasis?
Most people who have taeniasis don’t have any symptoms. If signs and symptoms are present, they may include:
- pain
- unexplained weight loss
- blockage of the intestine
- digestive problems
Some people with taeniasis may also experience irritation in the perianal area, which is the area around the anus. Worm segments or eggs being expelled in the stool cause this irritation.People often become aware that they have a tapeworm when they see worm segments or eggs in their stool.Infections can take between 8 and 14 weeks to develop.
What causes taeniasis?
You can develop taeniasis by eating raw or undercooked beef or pork. Contaminated food can contain tapeworm eggs or larvae that grow in your intestines when eaten.Fully cooking beef or pork will destroy the larvae so that they can’t live in your body.The tapeworm can grow up to 12 feet in length. It can live in the intestines for years without being discovered. Tapeworms have segments along their bodies. Each of these segments can produce eggs. As the tapeworm matures, these eggs will be passed out of the body in the stool.
Poor hygiene can also cause the spread of taeniasis. Once tapeworm larvae are in human stool, they can be spread through contact with the stool. You should wash your hands properly to help prevent the spread of the infection.
What are the risk factors for taeniasis?
Taeniasis is more commonTrusted Source in areas where raw beef or pork is consumed and where sanitation is poor. These areas may include:
- Eastern Europe and Russia
- East Africa
- sub-Saharan Africa
- Latin America
- parts of Asia, including China, Indonesia, and South Korea
Taeniasis is more likely to develop in people who have weakened immune systems and aren’t able to fight off infections. Your immune system can weaken due to:
- HIV
- AIDS
- an organ transplant
- diabetes
- chemotherapy
How is taeniasis diagnosed?
See your doctor if you see worm segments or eggs in your stool. Your doctor will ask you about your health history and recent travel outside of the United States. Doctors will often be able to make a diagnosis of taeniasis based on the symptoms.
To confirm the diagnosis, your doctor may order blood tests including a complete blood count (CBC). They may also order a stool exam to see if eggs or worm segments are present.
How do you get rid of a tapeworm?
Taeniasis is typically treated with medications prescribed by your doctor. Medications for the treatment of taeniasis include praziquantel (Biltricide) and albendazole (Albenza).Both drugs are antihelmintics, which means that they kill parasitic worms and their eggs. In most cases, these medications are provided in a single dose. They can take a few weeks to fully clear an infection. The tapeworm will be excreted as waste.Common side effects associated with these medications include dizziness and upset stomach.
What is the outlook for people with taeniasis?
Most cases of this infection go away with treatment. Medications prescribed for this condition are typically effective and will cure the infection.
What complications are associated with taeniasis?
In rare cases, serious complications from the infection can occur. Tapeworms may block your intestines. This may require surgery to correct.In other cases, a pork tapeworm may travel to other parts of your body such as the heart, eye, or brain. This condition is called cysticercosis. Cysticercosis can cause other health problems such as seizures or infections in the nervous system.
How can taeniasis be prevented?
The most effective way to prevent taeniasis is to cook food thoroughly. This means cooking meat to a temperature above 140°F (60°F) for five minutes or more. Measure the meat temperature with a cooking thermometer.After cooking meat, allow it to stand for three minutes before cutting it. This can help destroy any parasites that may be in the meat.
DR MN SINGH, HEAD, EPIDEMIOLOGY, TMH
REFERENCE-ON REQUEST
IMAGE-CREDIT-GOOGLE