Cesarean Section In Cow & Buffalo
Dr Uday Kumar , Veterinary Surgeon ,NIPER, Hazipur
Indications:-
Various types of dystocia, including those caused by relative fetal oversize when the pelvic inlet in young heifers is too small to allow delivery, deformities of the maternal pelvis, fetal monstres, induration of the cervix, fetal malposition, hydrops amnii and allantois, uterine torsion, and emphysematus fetuses. Fetal muscular hypertrophy “double muscling” in which the fetal hips and buttocks have the greatest transverse diameters of all fetal parts.
Cesarean section is clearly indicated when the uterus is ruptured in order to avoid further trauma to the uterus, major uterine vessels and small intestines.
Different approaches are indicated in various dystocia situations. The left paralumbar or flank approach is the standard incision for a viable or recently expired uncontaminated fetus and a cow that is capable of tolerating surgery while standing. In some situations, right flank laporatory is indicated if there is marked distention of the rumen or when clinical examination dictate that removal from the right side would be more convenient. For example, an oversized fetus situated in the right side of the abdominal cavity would be difficult to remove by left-flank incision. In the routine case, however, the left-flank incision is more convenient because fewer problems with encroaching intestines are encountered. The right-flank approach has also been recommended for hydrops cases.In the case of a dead and emphysematous fetus, a ventral approach should be used, or ventrolateral oblique approach, which may be performed with the animal in lateral recumbency. Both techniques reduce contamination of the peritoneum, which may occure during removal of the emphysematous, contaminated fetus and its associated debris. The ventral approaches are also indicated if the animal is recumbent and considered incapable of standing during surgery.
Anesthesia and surgical preparation:
Local analgesia. If the flank approach is used, a paravertebral block, inverted L block or a line block may be used. For paramedian approach, a high epidural, inverted L block, or line block may be used.
The surgical area is prepared for aseptic operation.
Surgical technique:
One) Flank approach, the incision is usually made more venteral in the flank.
Two) The ventral paramedian incision is midway between the midline and the subcutaneous abdominal vein and extends from the umbilicus caudal to the mammary gland. Following entrance into the peritoneal cavity, the surgeon manipulates a portion of the uterine horn containing the fetus and attempts to exteriorize an area for hysterotomy. The uterine incision is usually made over a limb, but in certain malpositions, the area over the head may be incised. Such exteriorization would not be possible with a swollen, emphysematous fetus. In these cases, the need for a ventral approach in which the uterus can be apposed more closely to the incision is obvious. The incision needs to be long enough to allow removal of the fetus without further tearing or extending the uterine incision. An attempt should also be made to avoid incising caruncles. The fetus is then removed with the surgeon attempting to retain the uterus so that the fetal fluids do not fall back into the peritoneal cavity.
Antibiotic tablets are inserted in the uterus perior to its closure. The uterus is closed with a continuous inverting pattern with No. 3 chromic guet. After the uterus is closed, it is replaced in position. The laparotomy incision is closed as usual.
Post operative management:
Antibiotics are administered. Oxytocin may be injected after uterine closure to enchance uterine involution.
𝘾𝙖𝙚𝙨𝙖𝙧𝙚𝙖𝙣 𝙨𝙚𝙘𝙩𝙞𝙤𝙣 (𝙝𝙮𝙨𝙩𝙚𝙧𝙤𝙩𝙤𝙢𝙮)
𝙄𝙣𝙙𝙞𝙘𝙖𝙩𝙞𝙤𝙣𝙨
• relative foetal oversize: immaturity of dam, double muscling (e.g. Belgian Blue), genetic mismatching and prolonged gestation (certain sires)
• foetal deformity (e.g. schistosoma reflexus; ankylosis)
• relative or absolute narrowness of the pelvic canal:immaturity of the dam, traumatic pelvic deformity, e.g. fracture
• foetal emphysema with a narrow birth canal
• foetal malpresentation or posture
• irreducible uterine torsion, uterine rupture
• atresia or hypoplasia of the maternal vagina or vulva
• certain valuable pedigree breeding programmes where safe delivery of a viable foetus is paramount and where management precludes the risks associated with a natural delivery
•over-fatdam,particularlyprimiparousheifers,resulting ina narrow pelvic canal and a high risk of vaginal tea
𝘾𝙤𝙣𝙩𝙧𝙖-𝙞𝙣𝙙𝙞𝙘𝙖𝙩𝙞𝙤𝙣𝙨
The following will decrease the chance of cow survival:
• cattle in very poor bodily condition(cachectic)
• emphysematous foetus
• uterine infection
𝘼𝙙𝙫𝙖𝙣𝙩𝙖𝙜𝙚𝙨 𝙤𝙛 𝙖 𝙘𝙖𝙚𝙨𝙖𝙧𝙚𝙖𝙣 𝙨𝙚𝙘𝙩𝙞𝙤𝙣 𝙤𝙫𝙚𝙧
• if the foetus is alive
• often faster and safer
• feasible procedure where embryotomy would be impossible (e.g. cervical
𝙁𝙡𝙖𝙣𝙠 𝙖𝙥𝙥𝙧𝙤𝙖𝙘𝙝
Restraint, preparation and anaesthesia
•a standing patient is preferable
• xylazine sedation is contra-indicated due to an induced increase of myo metrial tone and uterine friability, which makes suturing more difficult; also a higher risk of sudden recumbency. However, safety considerations sometimes necessitate sedation
• a uterine relaxant (e.g. clenbuterol HCl) can be slowly injected i.v. to facilitate rotation and partial exteriorisation of the uterus (300–450 μg, depending on the size of the cow)
• administer pre-operative systemic pain relief (NSAIDs)
•if anti biotics are to be used (asisusual), administera pre-operative systemic dose, e.g. amoxycillin or penicillin plus streptomycin i.m.
• caudal epidural anaesthesia (to reduce abdominal straining and rumen prolapsing through incision) is optional; 1ml of local anaesthetic per 100kg bodyweight is usually sufficient to reduce straining
𝙏𝙚𝙘𝙝𝙣𝙞𝙦𝙪𝙚
• clip, scrub and disinfect the entire paralumbar fossa (last rib to hip); use of sterile drapes is optional (often difficult to use practically in a standing patient)
• make a 30–35cm vertical incision in the middle or caudal third of the left paralumbarfossa incise through theskin only,using a scalpel
•muscle depth can vary considerably between patients(30mmto >100mm); avoid a scalpel; dissect at one point to penetrate the peritoneum (obvious influx of air into the abdominal cavity) before extending the incision ventrally and dorsally; take care not to incise the rumen wall
• haemostasis of the flank vessels isoptional; sharpand blunt dissection of the muscle layers using scissors reduces bleeding
• insert a hand into the abdomen, pushing the rumen forward and feeling
ventrally and caudally
• make a rapid assessment of the foetal position and the condition of the
uterine wall
• bring a greater curvature of the gravid horn towards the abdominal incision by gently but firmly lifting the foetus within the uterus; this is easier if pregnancy is in the left horn
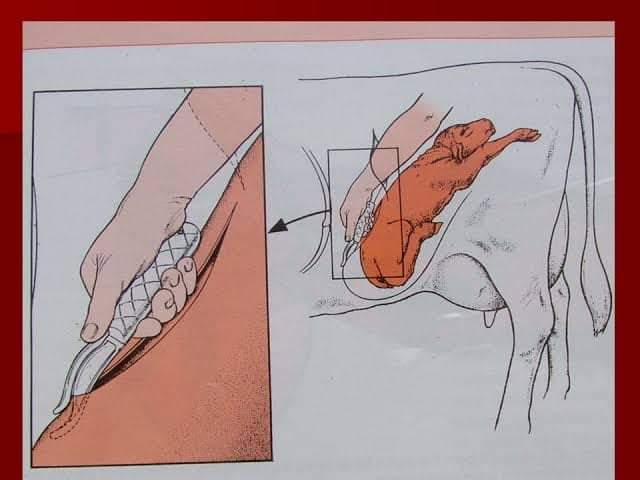
•grasp the uterine wall over the protruding part of the foetus(e.g.limb,hock in anterior presentation) and exteriorise greater curvature of the gravid
horn; if the dorsum of the foetus is towards the incision, the uterus should be rotated within the abdomen
• grasp a foetal leg just below the hock through the uterine wall and maintain firmly in a flank incision; grasp the fore limb below the carpus if the foetus is in a posterior presentation
•incisetheuterinewall(seeFigure6.1)alongthegreatercurvatureadjacent to the limb and towards the tip of the horn with scissors or a finger embryotomy (fetotomy) knife starting at the hock and extending towards the digits (or begin at the carpus in the fore limb, if in a posterior presentation)
• avoid incising maternal caruncles; avoid a scalpel to reduce the risk of
damaging the calf
• extend the incisioncarefully until the limb can be exteriorised without risk
of tearing the uterine wall
•manuallydissectthroughthefoetalmembranestofullyexteriorisethefoot; foetal fluids will begin to drain externally
• if necessary, instruct the assistant to maintain a very gentle traction on theexteriorisedlimbsuficient to maintain the uterine wall in the flank incision
• locatethesecondlimbthroughtheuterine incisionand foetalmembranes, which is similarly exteriorised; attachment of sterile calving ropes is optional
• ensure that foetal traction is applied gently and in the appropriate direction, usually initially upwards, the ventrally and caudally;lengthen the uterine incision, if required, with scissors to avoid any spontaneous tearing of the uterine wall
• practise careful and slow foetal manipulation during extraction, especially in cases of schistosoma reflexus, muscle contracture and emphysematous calves, to avoid uterine tears
• in case of gross foetal oversize or ankylosis the skin incision may occasion ally require enlargement to 40cm
• permit the umbilical cord to rupture naturally during extraction
• after delivery hold the uterine incision in the flank wound; manually remove any loose protruding portions of the placenta, leaving the remain der in situ
• do not attempt to separate the placenta frommaternal caruncles; trimming with scissors may be necessary
• non-crushing uterine clamps (vulsellum forceps) can be used to hold the uterus In position
• intrauterine medication is unnecessary
• while the foetus is being revived and the umbilical cord is checked, undertake uterine repair rapidly
• close the uterus with a continuous Cushing suture, followed by a continu ous Lembert or a modified Cushing (Utrecht uterine suture with buried knots)
• sutures should incorporate serosa and muscularis, but not perforate mucosa (risk of contamination); suture knots should be buried
• suture of the uterine wall: start at the caudal ventral commissure of the wound if a single layer closure is intendedor cranially if two layers are tobe inserted
.Suturematerial:either 5or6 metric PGA, polyglactinor 7 metric chromic catgut
• swab the incision after closure and check for leaks; rapid uterine contrac
Reference-On Request